“If we knew what it was we were doing, it would not be called research, would it?” Albert Einstein
Part One
I’m often asked if I think statin drugs are useful. Of course it’s important first to address the issue of cholesterol levels which statin drugs are used to control. I recently wrote a blog entitled “What can Centenarians teach us about cholesterol levels and longevity – It isn’t what you think” in which I provided substantial evidence questioning the current guidelines regarding what is actually a healthy total cholesterol level.
As far as statins go, my opinion is that if people are willing to be involved in their own healthcare by adopting a comprehensive approach to health optimization—which includes a healthy diet and lifestyle, the support of appropriate botanical and nutritional medicines, and a positive attitude—then I see little to no need for statin drugs.
However, if you do feel the need to take a statin, then I will provide you with essential supportive care to both mitigate the adverse effects of statins and to potentiate them, so that a reduced amount might be sufficient.
Statins Can Cause Harm for Some People
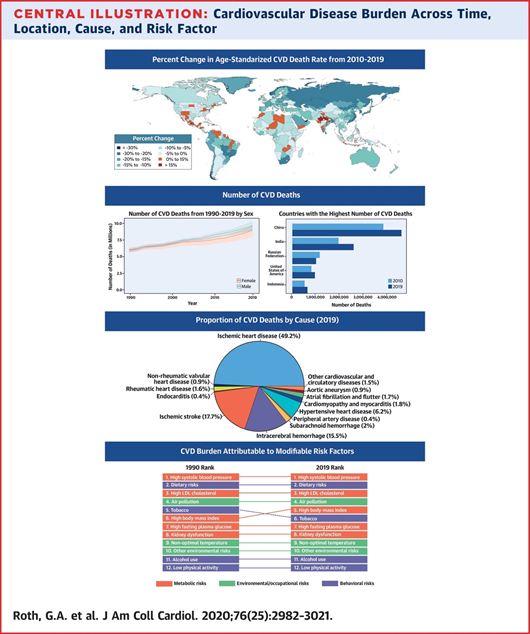
Despite the increased use of statins and other cardiovascular drugs over the last 30 years, deaths and disability from cardiovascular disease have been steadily rising across the globe. In 2019, cardiovascular disease, which includes heart disease and stroke, was responsible for a staggering one-third of all deaths worldwide.[1]
For some people, statin drugs do more harm than good. In a study that examined data from over two million patients, including over 225,000 patients who were new statin drug users, researchers found that for every 10,000 women treated with statins, there were only 271 fewer cases of heart disease. At the same time, the statins caused 74 cases of liver damage, 23 cases of acute kidney failure, 39 cases of extreme muscle weakness and 307 cases of cataracts. Statin drugs, in other words, helped 271 people but harmed 443 people. This demonstrates how statins are wreaking havoc with the health of those who take them causing damage that far outweighs any benefit they might offer.[2]
Statins are the most widely used drugs for treating hyperlipidemia. Although these drugs are purported to be safe, many patients taking them suffer from myopathy (muscle weakness). [3],[4],[5],[6],[7] This is concerning, because the heart is a muscle that never stops working in its job of pumping blood throughout the body. Statin-associated muscular symptoms range from asymptomatic elevation of serum creatine kinase (CK) to life-threatening rhabdomyolysis.[8] Several molecular mechanisms underlie statin-induced myopathy, including a decrease in levels of essential mevalonate and cholesterol derivatives.[9]
Skeletal muscle-associated symptoms (SAMS) are a frequent reason for stopping treatment with statins. Common SAMS include fatigue, weakness and pain, possibly accompanied by elevated serum creatine kinase activity. The most severe muscular adverse reaction is the potentially fatal rhabdomyolysis, which is whole-scale muscle breakdown. In most cases, rhabdomyolysis occurs following the use of these drugs for at least one week. But cases of rhabdomyolysis after just a single dose of simvastatin have been reported.44

The frequency of SAMS is variable but occurs in up to 30% of patients taking statins.[10]
The Effect of Statins on COQ-10 Levels and Mitochondria
Mitochondria are the tiny “engines” of our cells. Studies show that statins have several negative effects on mitochondria, including reduction of coenzyme Q10 levels, inhibition of respiratory chain complexes, induction of mitochondrial apoptosis, and dysregulation of Ca2+ metabolism and carnitine palmitoyltransferase-2 expression.
Treatment with statin drugs is associated with mitochondrial oxidative stress, which activates apoptosis and contributes to myopathy. Glycolytic muscles are more sensitive to atorvastatin than oxidative muscles, likely because of the higher antioxidative capacity in oxidative muscles.[11] Statin-induced myopathy (SIM) is a secondary mitochondrial myopathy,[12] since statins exhibit their side effects mainly by interaction with mitochondria.[13]
A deficiency of CoQ10 has been linked to congestive heart failure (CHF), which is a leading cause of morbidity and mortality in the elderly and accounts for more hospitalizations than any other condition. A 2-year, multicenter study of 420 patients with moderate to severe CHF showed that adding CoQ10 (100 mg three times daily) to conventional drug therapy reduced CV mortality by 42% and all-cause mortality by 44%. It also reduced CHF-related hospitalizations.[14]
Advanced stages of CHF can be associated with serious complications such as cardiac cachexia (defined as unintentional weight loss of more than 6 % in 6 months). Cardiac cachexia and the associated progressive weight loss are sometimes overlooked by older patients, their families and care providers.[15] Statins also reduce exercise capacity, and long-term use can lead to decreased skeletal muscle strength and increased risk of falling in elderly patients.[16]
Statin-related side effects, including statin cardiomyopathy, are far more common than previously recognized. However, these side effects are reversible with the combination of statin discontinuation and supplemental CoQ10 and other mitochondrial-enhancing nutrients and botanicals.Ubiquinol, the reduced form of CoQ10, has significantly higher absorption and bioavailability than non-reduced form (ubiquinone), making it the best choice for people with chronic inflammation or an inflamed digestive tract.
Neuroendocrine and Endocrine Abnormalities are a Major Contributor to Cardiac Cachexia and Statin-Induced Myopathy (SIM)
Impaired cardiac function is linked to general neurohormonal activation via stimulation of the sympathetic nervous system, the renin-angiotensin-aldosterone axis and the natriuretic peptide system. At the onset of cardiac heart failure, these systems are thought to be beneficial, but they contribute to increased vascular resistance and afterload, ventricular enlargement, and remodeling. The neurohormonal hypothesis postulates that heart failure progresses as a result of activation of endogenous neurohormonal systems, which exert deleterious effects on the heart and circulation.[17]
Research shows that the stress hormone cortisol is part of the general stress response with a catabolic action increased manifestly (2.5-fold) in untreated CHF patients with severe disease and particularly in cachectic CHF patients.[18] The clinical severity of CHF illness corresponds to the degree of the increase in resting energy demands. Plasma norepinephrine may reflect overall sympathetic activity.[19]
Statin drugs, such as Simvastatin induce myotube atrophy and cell loss that is associated with impaired ADP-stimulated maximal mitochondrial respiratory capacity, mitochondrial oxidative stress, and apoptosis in primary human skeletal myotubes, suggesting that mitochondrial dysfunction may underlie human statin-induced myopathy. SIM suggests a correlation with impairment of mitochondrial function. Long-term treatment with statin drugs increases respiration and the production of superoxide in mitochondria of peripheral blood mononuclear cells (PBMCs) and platelets.[20]

Along with lowering low-density lipoprotein cholesterol (LDL-C) levels, statin therapy can decrease the levels of serum steroid hormones, including testosterone and cortisol. [21],[22] Low testosterone in men is a major risk factor for cardiovascular disease and has other deleterious effects, including erectile dysfunction.[23],[24] Adding to the problem is that many men aromatize (convert) their testosterone into estrogen, and elevated estrogen in men is a cardiovascular risk factor as well. Yet, treating men with testosterone not only does not help, it appears to increase this risk.
Instead of prescribing hormones, my philosophy is to restore Essence, which is the reservoir from which we create hormones. This is accomplished through dietary and lifestyle support, as well as through the use of specific herbs that nourish and restore vitality.
Additional Risks of Statin Use: Diabetes, Cognitive Decline, and Dementia
In addition to muscular and cardiovascular risks, the use of statins has been associated with the onset of pathological conditions like diabetes and dementia. This is a result of interference with mitochondrial pathways by various mechanisms, such as reduction in mitochondrial oxidative phosphorylation, increase in oxidative stress, decrease in uncoupling protein 3 concentration, and interference in amyloid-β metabolism.[25]
The US Food and Drug Administration (FDA) now requires labeling requirements for statins to include a warning about the possibility of increased blood sugar and HbA1c levels and the European Medicines Agency to issue guidance on a small increased risk of T2D with the statin class.[26]
In recent years, several randomized, controlled trials and observational studies have reported increased risk for new-onset type 2 diabetes mellitus (T2D) with statin treatment, particularly with use of high-intensity statins that reduce LDL-C by 50% or more.[27].[28],[29]
Taking statin drugs also appears to reduce cognitive function. Researchers in the journal Pharmacotherapy reported two women who experienced significant cognitive impairment temporally related to statin therapy. One woman took Atorvastatin, and the other first took Atorvastatin, then was rechallenged with Simvastatin. The researchers warned that clinicians should be aware of cognitive impairment and dementia as potential adverse effects associated with statin therapy.[30]

A larger study observed 283 people—94 in the placebo group, 96 in the 10-mg Simvastatin group, and 93 in the 40-mg Simvastatin group. Compared with the placebo, Simvastatin was associated with minor negative changes in performance on several tests assessing attention, memory, and overall mental efficiency. In the team’s earlier trial, 20 mg of Lovastatin given every day for six months produced similar changes on the same tests.[31]
A survey by the MedWatch drug surveillance system of the Food and Drug Administration (FDA) from November 1997-February 2002 for reports of statin-associated memory loss identified 60 patients who had memory loss associated with statins. About 50% of the patients noted cognitive adverse effects within 2 months of therapy. Fourteen (56%) of 25 patients noted improvement when the statin was discontinued. There are no available prospective studies that show cognitive or anti-amyloid benefits for any statin, although some people are actually touting statins to be beneficial for the prevention of dementia.[32]
Statin-Related Autoimmune Myopathy
Recently, our understanding of statin-associated myopathy has expanded to include not only a toxic myopathy with limited and reversible side-effects but also an autoimmune variety. In this case, statins likely induce an autoimmune myopathy that is both associated with a specific autoantibody and is responsive to immunosuppression and immune modulation.
Statin-associated immune-mediated myopathy provides an example of an environmental trigger (statins) directly implicated in an autoimmune disease associated with a genetic predisposition as well as potential risk factors including concomitant diseases and specific statins.[33]
What Really Causes Vascular Disease?
Diseases of the vascular system have long been considered to be age-related in terms of their onset and progression.[34] Although there is a small amount of truth with regard to the role lipid balance plays in health as one ages, it is no more important than oxidative damage and glutathione-dependent redox homeostasis. Cardiovascular disease is most often caused by a chain of effects that increase catabolic activity while decreasing anabolic activity. This includes hormone dysfunction/imbalance (loss of testosterone, DHEA, growth hormone, or elevated cortisol and/or insulin), key receptors and enzymes, pro-inflammatory and oxidative damage, elevated fibrinogen, and mitochondrial atrophy.
Atherosclerosis, the main cause of cardiovascular disease, is a chronic inflammatory condition[35] that associated with an overproduction of oxidant species, namely peroxynitrite, which is a powerful oxidant that reacts directly with all biomolecules. Glutathione is an efficient scavenger of peroxynitrite, so, modulation of glutathione synthesis may provide a strategy to selectively protect cells from this oxidant. Higher levels of plasma glutathione are associated with a lower incidence of cardiovascular disease.[36]
Abnormalities in intracellular GSH cycling are associated with increased lipid peroxidation in congestive heart failure.[37] Also, reduced sulfur-containing amino acid alterations have been found in the progression of chronic ischemic heart disease to heart failure status, as an additional pro-oxidant stimulus for worsening oxidative stress.[38]
A key role for glutathione-dependent redox homeostasis is the preservation of telomere function in endothelial cells. Loss of telomere integrity is a major trigger for the onset of premature aging under mild chronic oxidative stress. The telomeres contain condensed DNA material, giving stability to the chromosomes.[39]
Glutathione is formed in the body from three amino acids (cysteine, glycine, and glutamic acid), and forms a part of the antioxidant enzyme glutathione peroxidase. Undenatured whey protein concentrate (WPC), which is rich in cysteine, raises glutathione levels. Many natural compounds and herbs either enhance glutathione production or spare the breakdown of glutathione, enabling it to recycle and inhibit the oxidation of glutathione.
A family of compounds called isothiocyanates, including 2-phenethyl isothiocyanate and sulforaphane (SFN) derived from cruciferous vegetables such as broccoli sprouts, activate glutathione, reduce oxidative damage, and aid in detoxification of environmental carcinogens and toxicants. Isothiocyanates act via cytoplasmic Nrf2 to enhance the production of redox-antioxidants throughout the body through the glutathione pathway.[40],[41]
A recent meta-analysis and systematic review of SFN on lipid reduction and weight control assessed mice and rats fed a high-fat diet. SFN supplements decreased the level of body weight and significantly improved lipid profiles in rodents.
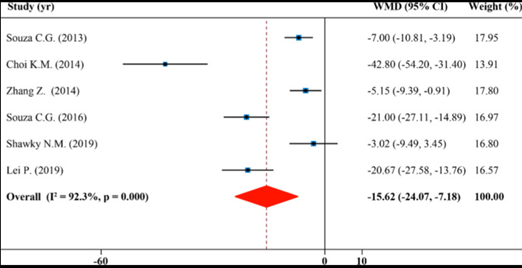
Forest plot showing effects of SFN on serum total cholesterol
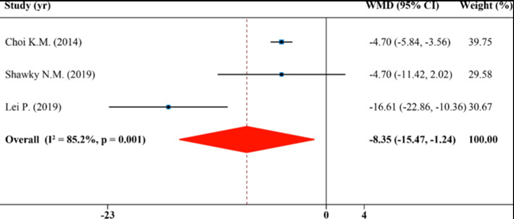
Forest plot showing effects of SFN on serum low-density lipoprotein cholesterol[42]
Selenium (Se) is an integral part of the enzyme glutathione, one of the central players of the heart’s redox-antioxidant system, and a deficiency is implicated in certain types of heart disease. Myocardial oxidative stress in chronic heart failure may be augmented at least in part by concomitant glutathione deficiency, and the administration of Se could rescue the exhaustion of this selenoprotein, resulting in improved left ventricular function.[43]
“Science without religion is lame, religion without science is blind.”
- Albert Einstein
The Mediterranean Diet as an Alternative to Statins
Statins are not the only anti-atherosclerosis treatments available. Many studies have demonstrated that the Mediterranean diet offers significant protection from heart disease and cancer, and substantially increases lifespan.Several of these recent studies have shown that eating a Mediterranean diet decreases the absolute risk reduction (ARR) of CAD values more effectively than using statin drugs.[44],[45],[46],[47],[48],[49]
The Mediterranean diet includes locally grown wild vegetables, as well other common vegetables, such as cabbage, leafy and root vegetables, bitter greens (including arugula, radicchio, endive), mushrooms, tomatoes and other fruiting vegetables, grapes and berries, fish, a moderate intake of hard cheeses, grains, and plenty of olive oil.
Greater adherence to the Mediterranean diet is associated with significant reduction in overall mortality, mortality from cardiovascular diseases and stroke, incidence of or mortality from cancer, and incidence of Parkinson’s disease and Alzheimer’s disease and mild cognitive impairment.[50] For those taking statins, reducing simple carbohydrates, eating whole foods, and adherence to a high‐fiber diet have been shown to resolve manifestations of SIM.[51]
A 2020 Cochrane meta-analyses (41 total reports) of randomized clinical trials revealed a beneficial effect of the Mediterranean diet on total CVD incidence.[52]
A 2016 study of more than 20,000 adults found that people who follow a Mediterranean diet are much less likely to develop heart disease,and the researchers estimated that up to 4% of all heart disease cases could be prevented with adherence to a Mediterranean diet.[53]
Another study looked at the risk of heart attack, stroke, and death from cardiovascular causes between people who followed a Mediterranean diet and people who did not. The study, which lasted nearly five years, concluded that the risks were about 30 percent lower in people who followed a Mediterranean diet.[54]
If you’re still not convinced that the Mediterranean diet is heart-healthy, check out this 2019 review of studies, which looked at 29 individual studies on the Mediterranean diet. The authors of the review concluded that the Mediterranean diet is protective against various forms of heart disease.[55]
Adopting a Mediterranean diet after a heart attack is almost three times as powerful in reducing mortality as taking a statin. The recently published PREDIMED randomized controlled trial was stopped early after it showed that in high-risk people, the Mediterranean diet achieved a 30% improvement over a “low fat” diet in terms of cardiovascular events.[56]
Lastly, exercise is an effective therapy to prevent metabolic and cardiovascular diseases and may also help to mitigate SIM.[57]
God embraces you as you are—shadow and light, everything. God embraces it, by grace. —Brother David Steindl-Rast
The Importance of Attitude in Health
In the management of health and the prevention of disease, our focus tends to be on drugs (from a conventional perspective) or foods and supplements (from a more natural, health supportive perspective). While I am a strong proponent of a healthy diet and botanical and nutritional supplements, I also believe that we cannot achieve optimal health without attention to attitude.
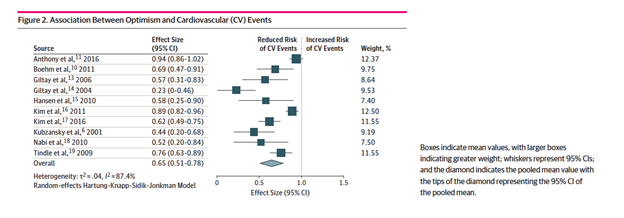
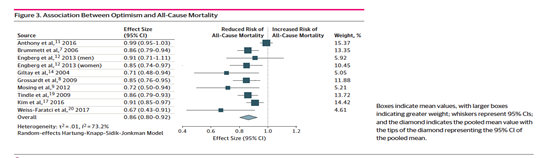
When one the last time your health-care practitioner talked with you about attitude and health? Did you know that optimism is associated with a significant reduction in cardiovascular events and all-cause mortality according to a systematic review and meta-analysis?
[1] Gregory A. Roth George A. MensahCatherine O. Johnson, Giovanni Addolorato, Enrico Ammirati, Larry M. Baddour, Noël C. Barengo, Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study, J Am Coll Cardiol. 2020 Dec, 76 (25) 2982–3021, https://www.jacc.org/doi/pdf/10.1016/j.jacc.2020.11.010
[2] Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ. 2010 May 20;340:c2197. doi: 10.1136/bmj.c2197.
[3] Phillips PS, Haas RH.Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2003 Jun 17;138(12):1008-9. Scripps Mercy Hospital; San Diego, CA 92103
[4] Jamil S, Iqbal P. Rhabdomyolysis induced by a single dose of a statin. Heart. 2004 Jan;90(1):e3. Medical Directorate, Chesterfield and North Derbyshire Royal Hospital NHS Calow, Chesterfield, UK
[5] Chang JT, Staffa JA, Parks M, Green L. Rhabdomyolysis with HMG-CoA reductase inhibitors and gemfibrozil combination therapy.Pharmacoepidemiol Drug Saf. 2004 Jul;13(7):417-26. Office of Drug Safety, Food and Drug Administration, Rockville, MD 20857, USA. changJ@cder.fda.gov
[6] Bellosta S, Paoletti R, Corsini A. Safety of statins: focus on clinical pharmacokinetics and drug interactions. Circulation. 2004 Jun 15;109(23 Suppl 1):III50-7., Department of Pharmacological Sciences, University of Milan, Milan, Italy.
[7] Langsjoen PH, Langsjoen JO, Langsjoen AM, Lucas LA. Treatment of statin adverse effects with supplemental Coenzyme Q10 and statin drug discontinuation. Biofactors. 2005;25(1-4):147-52.
[8] Stroes E.S., Thompson P.D., Corsini A., Vladutiu G.D., Raal F.J., Ray K.K., Roden M., Stein E., Tokgözoğlu L., Nordestgaard B.G., et al. Statin-associated muscle symptoms: Impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur. Heart J. 2015;36:1012–1022. doi: 10.1093/eurheartj/ehv043
[9] Ahmadi Y, Ghorbanihaghjo A, Naghi-Zadeh M, Yagin NL. Oxidative stress as a possible mechanism of statin-induced myopathy. Inflammopharmacology. 2018 Jun;26(3):667-674. doi: 10.1007/s10787-018-0469-x. Epub 2018 Mar 24. PMID: 29574631.
[10] Bouitbir J, Sanvee GM, Panajatovic MV, Singh F, Krähenbühl S. Mechanisms of statin-associated skeletal muscle-associated symptoms. Pharmacol Res. 2020 Apr;154:104201. doi: 10.1016/j.phrs.2019.03.010. Epub 2019 Mar 12. PMID: 30877064.
[11] Bouitbir J, Singh F, Charles AL, Schlagowski AI, Bonifacio A, Echaniz-Laguna A, Geny B, Krähenbühl S, Zoll J. Statins Trigger Mitochondrial Reactive Oxygen Species-Induced Apoptosis in Glycolytic Skeletal Muscle. Antioxid Redox Signal. 2016 Jan 10;24(2):84-98. doi: 10.1089/ars.2014.6190. PMID: 26414931.
[12] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36.
[13] Schirris TJ, Renkema GH, Ritschel T, Voermans NC, Bilos A, van Engelen BG, Brandt U, Koopman WJ, Beyrath JD, Rodenburg RJ, Willems PH, Smeitink JA, Russel FG. Statin‐induced myopathy is associated with mitochondrial complex III inhibition. Cell Metab 2015;22:399–407
[14] Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D, Alehagen U, Steurer G, Littarru GP; Q-SYMBIO Study Investigators. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014 Dec;2(6):641-9. doi: 10.1016/j.jchf.2014.06.008. Epub 2014 Oct 1. PMID: 25282031.
[15]Azhar, G., Wei, J.Y. New Approaches to Treating Cardiac Cachexia in the Older Patient. Curr Cardiovasc Risk Rep 7, 480–484 (2013). https://doi.org/10.1007/s12170-013-0353-6
[16] Kwak HB, Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014 Sep; 4(2):71-9.
[17] Wolfram Steinborn and Stefan D. Anker, Cardiac Cachexia: Pathophysiology and Clinical Implications, Basic Appl Myol 13 (4): 191-201, 2003
[18] Packer M: The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol 1992; 20: 248-254.
[19] Obisesan TO, Toth MJ, Donaldson K, Gottlieb SS, Fisher ML, Vaitekevicius P, Poehlman ET: Energy expenditure and symptom severity in men with heart failure. Am J Cardiol 1996; 77: 1250-1252.
[20] Durhuus JA, Hansson S, Morville T, Kuhlman AB, Dohlmann TL, Larsen S, Helge JW, Angleys M, Muniesa-Vargas A, Bundgaard JR, Hickson ID, Dela F, Desler C, Rasmussen LJ. Simvastatin improves mitochondrial respiration in peripheral blood cells. Sci Rep. 2020 Oct 12;10(1):17012. doi: 10.1038/s41598-020-73896-2. PMID: 33046789; PMCID: PMC7550337.
[21] Nakayama A, Morita H, Kawahara T, Itoh H, Komuro I. Association between testosterone and lipid profiles under statin therapy and its clinical impact on the cardiovascular event risk. Heart Vessels. 2021 May 26. doi: 10.1007/s00380-021-01872-5. Epub ahead of print. PMID: 34036416.
[22] Hsieh CJ, Huang B. Rosuvastatin decreases testosterone levels but not sexual function in men with type 2 diabetes. Diabetes Res Clin Pract. 2016 Oct;120:81-8. doi: 10.1016/j.diabres.2016.07.026. Epub 2016 Aug 6. PMID: 27525363.
[23] Baspınar O, Bayram F, Korkmaz S, Aksu M, Kocer D, Dizdar OS, Simsek Y, Toth PP. The effects of statin treatment on adrenal and sexual function and nitric oxide levels in hypercholesterolemic male patients treated with a statin. J Clin Lipidol. 2016 Nov-Dec;10(6):1452-1461. doi: 10.1016/j.jacl.2016.09.004. Epub 2016 Sep 13. PMID: 27919363.
[24] Bolat MS, Bakırtaş M, Fırat F, Akdeniz E, Çınar Ö, Erdemir F. The effect of atorvastatin on penile intracavernosal pressure and cavernosal morphology in normocholesterolemic rats. Turk J Urol. 2018 Aug 31;45(2):91-96. doi: 10.5152/tud.2018.98048. PMID: 30183612; PMCID: PMC6368041.
[25] Mollazadeh H, Tavana E, Fanni G, Bo S, Banach M, Pirro M, von Haehling S, Jamialahmadi T, Sahebkar A. Effects of statins on mitochondrial pathways. J Cachexia Sarcopenia Muscle. 2021 Apr;12(2):237-251. doi: 10.1002/jcsm.12654. Epub 2021 Jan 29. PMID: 33511728; PMCID: PMC8061391.
[26] Bilianou E, Carmena R, Ceška R, Corsini A, Erbel R, Flynn PD, Garcia-Moll X, Gumprecht J, Ishibashi S, Jambart S, Kastelein JJ, Maher V, da Silva PM, Masana L, Odawara M, Pedersen TR, Rotella CM, Salti I, Teramoto T, Tokgozoglu L, Toth PP, Valensi P, Vergès B. The use of statins in people at risk of developing diabetes mellitus: evidence and guidance for clinical practice. Atheroscler Suppl. 2014 Jun;15(1):1-15. doi: 10.1016/j.atherosclerosissup.2014.04.001. PMID: 24840509.
[27] Maki KC, Diwadkar-Navsariwala V, Kramer MW. Statin use and risk for type 2 diabetes: what clinicians should know. Postgrad Med. 2018 Mar;130(2):166-172. doi: 10.1080/00325481.2018.1402658. Epub 2017 Nov 22. PMID: 29139315. Sattar NA, Ginsberg H, Ray K, Chapman MJ, Arca M, Averna M, Betteridge DJ, Bhatnagar D,
[28] Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 2002;360:1623–1630.
[29] Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, et al. Statins and risk of incident diabetes: a collaborative meta‐analysis of randomised statin trials. Lancet 2010;375:735–742.
[30] King DS, Wilburn AJ, Wofford MR, Harrell TK, Lindley BJ, Jones DW. Cognitive impairment associated with atorvastatin and simvastatin. Pharmacotherapy. 2003 Dec;23(12):1663-7.
[31] Muldoon MF, Ryan CM, Sereika SM, Flory JD, Manuck SB. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am J Med. 2004 Dec 1;117(11):823-9.
[32] Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy. 2003 Jul;23(7):871-80.
[33] Christopher-Stine L, Basharat P. Statin-associated immune-mediated myopathy: biology and clinical implications. Curr Opin Lipidol. 2017 Apr;28(2):186-192. doi: 10.1097/MOL.0000000000000399. PMID: 28207435
[34] Lakatta, E. G. and Levy, D. (2003). Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation107, 139-146
[35] Kaplan RC, Frishman WH, Systemic inflammation as a cardiovascular disease risk factor and as a potential target for drug therapy. Heart Dis 2001 Sep-Oct;3(5):326-32.
[36] Haruki Shimizu, Yutaka Kiyohara, Isao Kato, Takanari Kitazono, Yumihiro Tanizaki, Michiaki Kubo, Hirofumi Ueno, Setsuro Ibayashi, Masatoshi Fujishima, and Mitsuo Iida, Relationship Between Plasma Glutathione Levels and Cardiovascular Disease in a Defined Population: The Hisayama Study, Stroke, Sep 2004; 35: 2072 – 2077.
[37] Campolo J, De Maria R, Caruso R, Accinni R, Turazza F, Parolini M, Roubina E, De Chiara B, Cighetti G, Frigerio M, Vitali E, Parodi O. Blood glutathione as independent marker of lipid peroxidation in heart failure. Int J Cardiol. 2007 Apr 12;117(1):45-50. Epub 2006 Aug 1
[38] Campolo J, Caruso R, De Maria R, Parolini M, Oliva F, Roubina E, Cighetti G, Frigerio M, Vitali E, Parodi O. Aminothiol redox alterations in patients with chronic heart failure of ischaemic or non-ischaemic origin. J Cardiovasc Med (Hagerstown). 2007 Dec;8(12):1024-1028.
[39] David J. Kurz1, Stephanie Decary, Ying Hong, Elisabeth Trivier, Alexander Akhmedov, Jorge D. Erusalimsky, Chronic oxidative stress compromises telomere integrity and accelerates the onset of senescence in human endothelial cells, Accepted 9 January 2004, Journal of Cell Science 117, 2417-2426
[40] Yuan JM, Murphy SE, Stepanov I, Wang R, Carmella SG, Nelson HH, Hatsukami D, Hecht SS. 2-Phenethyl Isothiocyanate, Glutathione S-transferase M1 and T1 Polymorphisms, and Detoxification of Volatile Organic Carcinogens and Toxicants in Tobacco Smoke. Cancer Prev Res (Phila). 2016 Jul;9(7):598-606. doi: 10.1158/1940-6207.CAPR-16-0032. Epub 2016 Apr 20. PMID: 27099270; PMCID: PMC4930697.
[41] Ladak Z, Garcia E, Yoon J, Landry T, Armstrong EA, Yager JY, Persad S. Sulforaphane (SFA) protects neuronal cells from oxygen & glucose deprivation (OGD). PLoS One. 2021 Mar 18;16(3):e0248777. doi: 10.1371/journal.pone.0248777. PMID: 33735260; PMCID: PMC7971874.
[42] Du K, Fan Y, Li D. Sulforaphane ameliorates lipid profile in rodents: an updated systematic review and meta-analysis. Sci Rep. 2021 Apr 8;11(1):7804. doi: 10.1038/s41598-021-87367-9. PMID: 33833347; PMCID: PMC8032686.
[43] Hiraoka Y. Association between function of selenium and heart disease, Nihon Rinsho. 2016 Jul;74(7):1192-8.
[44] Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA.Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004 Sep 22;292(12):1433-9.
[45] de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994 Jun 11;343(8911):1454-9. Erratum in: Lancet 1995 Mar 18;345(8951):738.
[46] de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999 Feb 16;99(6):779-85.
[47] Trichopoulou A, Bamia C, Trichopoulos D. Mediterranean diet and survival among patients with coronary heart disease in Greece. Arch Intern Med. 2005 Apr 25;165(8):929-35.
[48] Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, Manor O, Pella D, Berry EM. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002 Nov 9;360(9344):1455-61.
[49] de Lorgeril M, Salen P, Martin JL, Monjaud I, Boucher P, Mamelle N. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998 Jun 8;158(11):1181-7.
[50] Demarin V, Lisak M, Morović S. Mediterranean diet in healthy lifestyle and prevention of stroke. Acta Clin Croat. 2011 Mar;50(1):67-77.
[51] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36
[52] Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, Rahelić D, Sievenpiper JL, Salas-Salvadó J. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. 2020;60(7):1207-1227. doi: 10.1080/10408398.2019.1565281. Epub 2019 Jan 24. PMID: 30676058.
[53] Tong, T.Y.N., Wareham, N.J., Khaw, K. et al. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study. BMC Med 14, 135, (2016). https://doi.org/10.1186/s12916-016-0677-4
[54] Bailén Almorox R. Prevención primaria de la enfermedad cardiovascular con una dieta mediterránea [Cardiovascular disease primary prevention with a Mediterranean diet]. Rev Clin Esp (Barc). 2013 Oct;213(7):355-6. Spanish. doi: 10.1016/j.rce.2013.04.011. PMID: 24244956.
[55] Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173–191. doi:10.1007/s00394-017-1582-0.
[56] Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013 Apr 4;368(14):1279-90. doi: 10.1056/NEJMoa1200303. Epub 2013 Feb 25.
[57] Kwak HB. Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014;4(2):71-79. doi:10.15280/jlm.2014.4.2.71
Statin-Associated Myopathy and Mitochondrial Impairment
“If we knew what it was we were doing, it would not be called research, would it?” Albert Einstein
Part One
I’m often asked if I think statin drugs are useful. Of course it’s important first to address the issue of cholesterol levels which statin drugs are used to control. I recently wrote a blog entitled “What can Centenarians teach us about cholesterol levels and longevity – It isn’t what you think” in which I provided substantial evidence questioning the current guidelines regarding what is actually a healthy total cholesterol level.
As far as statins go, my opinion is that if people are willing to be involved in their own healthcare by adopting a comprehensive approach to health optimization—which includes a healthy diet and lifestyle, the support of appropriate botanical and nutritional medicines, and a positive attitude—then I see little to no need for statin drugs.
However, if you do feel the need to take a statin, then I will provide you with essential supportive care to both mitigate the adverse effects of statins and to potentiate them, so that a reduced amount might be sufficient.
Statins Can Cause Harm for Some People
Despite the increased use of statins and other cardiovascular drugs over the last 30 years, deaths and disability from cardiovascular disease have been steadily rising across the globe. In 2019, cardiovascular disease, which includes heart disease and stroke, was responsible for a staggering one-third of all deaths worldwide.[1]
For some people, statin drugs do more harm than good. In a study that examined data from over two million patients, including over 225,000 patients who were new statin drug users, researchers found that for every 10,000 women treated with statins, there were only 271 fewer cases of heart disease. At the same time, the statins caused 74 cases of liver damage, 23 cases of acute kidney failure, 39 cases of extreme muscle weakness and 307 cases of cataracts. Statin drugs, in other words, helped 271 people but harmed 443 people. This demonstrates how statins are wreaking havoc with the health of those who take them causing damage that far outweighs any benefit they might offer.[2]
Statins are the most widely used drugs for treating hyperlipidemia. Although these drugs are purported to be safe, many patients taking them suffer from myopathy (muscle weakness). [3],[4],[5],[6],[7] This is concerning, because the heart is a muscle that never stops working in its job of pumping blood throughout the body. Statin-associated muscular symptoms range from asymptomatic elevation of serum creatine kinase (CK) to life-threatening rhabdomyolysis.[8] Several molecular mechanisms underlie statin-induced myopathy, including a decrease in levels of essential mevalonate and cholesterol derivatives.[9]
Skeletal muscle-associated symptoms (SAMS) are a frequent reason for stopping treatment with statins. Common SAMS include fatigue, weakness and pain, possibly accompanied by elevated serum creatine kinase activity. The most severe muscular adverse reaction is the potentially fatal rhabdomyolysis, which is whole-scale muscle breakdown. In most cases, rhabdomyolysis occurs following the use of these drugs for at least one week. But cases of rhabdomyolysis after just a single dose of simvastatin have been reported.44
The frequency of SAMS is variable but occurs in up to 30% of patients taking statins.[10]
The Effect of Statins on COQ-10 Levels and Mitochondria
Mitochondria are the tiny “engines” of our cells. Studies show that statins have several negative effects on mitochondria, including reduction of coenzyme Q10 levels, inhibition of respiratory chain complexes, induction of mitochondrial apoptosis, and dysregulation of Ca2+ metabolism and carnitine palmitoyltransferase-2 expression.
Treatment with statin drugs is associated with mitochondrial oxidative stress, which activates apoptosis and contributes to myopathy. Glycolytic muscles are more sensitive to atorvastatin than oxidative muscles, likely because of the higher antioxidative capacity in oxidative muscles.[11] Statin-induced myopathy (SIM) is a secondary mitochondrial myopathy,[12] since statins exhibit their side effects mainly by interaction with mitochondria.[13]
A deficiency of CoQ10 has been linked to congestive heart failure (CHF), which is a leading cause of morbidity and mortality in the elderly and accounts for more hospitalizations than any other condition. A 2-year, multicenter study of 420 patients with moderate to severe CHF showed that adding CoQ10 (100 mg three times daily) to conventional drug therapy reduced CV mortality by 42% and all-cause mortality by 44%. It also reduced CHF-related hospitalizations.[14]
Advanced stages of CHF can be associated with serious complications such as cardiac cachexia (defined as unintentional weight loss of more than 6 % in 6 months). Cardiac cachexia and the associated progressive weight loss are sometimes overlooked by older patients, their families and care providers.[15] Statins also reduce exercise capacity, and long-term use can lead to decreased skeletal muscle strength and increased risk of falling in elderly patients.[16]
Statin-related side effects, including statin cardiomyopathy, are far more common than previously recognized. However, these side effects are reversible with the combination of statin discontinuation and supplemental CoQ10 and other mitochondrial-enhancing nutrients and botanicals.Ubiquinol, the reduced form of CoQ10, has significantly higher absorption and bioavailability than non-reduced form (ubiquinone), making it the best choice for people with chronic inflammation or an inflamed digestive tract.
Neuroendocrine and Endocrine Abnormalities are a Major Contributor to Cardiac Cachexia and Statin-Induced Myopathy (SIM)
Impaired cardiac function is linked to general neurohormonal activation via stimulation of the sympathetic nervous system, the renin-angiotensin-aldosterone axis and the natriuretic peptide system. At the onset of cardiac heart failure, these systems are thought to be beneficial, but they contribute to increased vascular resistance and afterload, ventricular enlargement, and remodeling. The neurohormonal hypothesis postulates that heart failure progresses as a result of activation of endogenous neurohormonal systems, which exert deleterious effects on the heart and circulation.[17]
Research shows that the stress hormone cortisol is part of the general stress response with a catabolic action increased manifestly (2.5-fold) in untreated CHF patients with severe disease and particularly in cachectic CHF patients.[18] The clinical severity of CHF illness corresponds to the degree of the increase in resting energy demands. Plasma norepinephrine may reflect overall sympathetic activity.[19]
Statin drugs, such as Simvastatin induce myotube atrophy and cell loss that is associated with impaired ADP-stimulated maximal mitochondrial respiratory capacity, mitochondrial oxidative stress, and apoptosis in primary human skeletal myotubes, suggesting that mitochondrial dysfunction may underlie human statin-induced myopathy. SIM suggests a correlation with impairment of mitochondrial function. Long-term treatment with statin drugs increases respiration and the production of superoxide in mitochondria of peripheral blood mononuclear cells (PBMCs) and platelets.[20]
Along with lowering low-density lipoprotein cholesterol (LDL-C) levels, statin therapy can decrease the levels of serum steroid hormones, including testosterone and cortisol. [21],[22] Low testosterone in men is a major risk factor for cardiovascular disease and has other deleterious effects, including erectile dysfunction.[23],[24] Adding to the problem is that many men aromatize (convert) their testosterone into estrogen, and elevated estrogen in men is a cardiovascular risk factor as well. Yet, treating men with testosterone not only does not help, it appears to increase this risk.
Instead of prescribing hormones, my philosophy is to restore Essence, which is the reservoir from which we create hormones. This is accomplished through dietary and lifestyle support, as well as through the use of specific herbs that nourish and restore vitality.
Additional Risks of Statin Use: Diabetes, Cognitive Decline, and Dementia
In addition to muscular and cardiovascular risks, the use of statins has been associated with the onset of pathological conditions like diabetes and dementia. This is a result of interference with mitochondrial pathways by various mechanisms, such as reduction in mitochondrial oxidative phosphorylation, increase in oxidative stress, decrease in uncoupling protein 3 concentration, and interference in amyloid-β metabolism.[25]
The US Food and Drug Administration (FDA) now requires labeling requirements for statins to include a warning about the possibility of increased blood sugar and HbA1c levels and the European Medicines Agency to issue guidance on a small increased risk of T2D with the statin class.[26]
In recent years, several randomized, controlled trials and observational studies have reported increased risk for new-onset type 2 diabetes mellitus (T2D) with statin treatment, particularly with use of high-intensity statins that reduce LDL-C by 50% or more.[27].[28],[29]
Taking statin drugs also appears to reduce cognitive function. Researchers in the journal Pharmacotherapy reported two women who experienced significant cognitive impairment temporally related to statin therapy. One woman took Atorvastatin, and the other first took Atorvastatin, then was rechallenged with Simvastatin. The researchers warned that clinicians should be aware of cognitive impairment and dementia as potential adverse effects associated with statin therapy.[30]
A larger study observed 283 people—94 in the placebo group, 96 in the 10-mg Simvastatin group, and 93 in the 40-mg Simvastatin group. Compared with the placebo, Simvastatin was associated with minor negative changes in performance on several tests assessing attention, memory, and overall mental efficiency. In the team’s earlier trial, 20 mg of Lovastatin given every day for six months produced similar changes on the same tests.[31]
A survey by the MedWatch drug surveillance system of the Food and Drug Administration (FDA) from November 1997-February 2002 for reports of statin-associated memory loss identified 60 patients who had memory loss associated with statins. About 50% of the patients noted cognitive adverse effects within 2 months of therapy. Fourteen (56%) of 25 patients noted improvement when the statin was discontinued. There are no available prospective studies that show cognitive or anti-amyloid benefits for any statin, although some people are actually touting statins to be beneficial for the prevention of dementia.[32]
Statin-Related Autoimmune Myopathy
Recently, our understanding of statin-associated myopathy has expanded to include not only a toxic myopathy with limited and reversible side-effects but also an autoimmune variety. In this case, statins likely induce an autoimmune myopathy that is both associated with a specific autoantibody and is responsive to immunosuppression and immune modulation.
Statin-associated immune-mediated myopathy provides an example of an environmental trigger (statins) directly implicated in an autoimmune disease associated with a genetic predisposition as well as potential risk factors including concomitant diseases and specific statins.[33]
What Really Causes Vascular Disease?
Diseases of the vascular system have long been considered to be age-related in terms of their onset and progression.[34] Although there is a small amount of truth with regard to the role lipid balance plays in health as one ages, it is no more important than oxidative damage and glutathione-dependent redox homeostasis. Cardiovascular disease is most often caused by a chain of effects that increase catabolic activity while decreasing anabolic activity. This includes hormone dysfunction/imbalance (loss of testosterone, DHEA, growth hormone, or elevated cortisol and/or insulin), key receptors and enzymes, pro-inflammatory and oxidative damage, elevated fibrinogen, and mitochondrial atrophy.
Atherosclerosis, the main cause of cardiovascular disease, is a chronic inflammatory condition[35] that associated with an overproduction of oxidant species, namely peroxynitrite, which is a powerful oxidant that reacts directly with all biomolecules. Glutathione is an efficient scavenger of peroxynitrite, so, modulation of glutathione synthesis may provide a strategy to selectively protect cells from this oxidant. Higher levels of plasma glutathione are associated with a lower incidence of cardiovascular disease.[36]
Abnormalities in intracellular GSH cycling are associated with increased lipid peroxidation in congestive heart failure.[37] Also, reduced sulfur-containing amino acid alterations have been found in the progression of chronic ischemic heart disease to heart failure status, as an additional pro-oxidant stimulus for worsening oxidative stress.[38]
A key role for glutathione-dependent redox homeostasis is the preservation of telomere function in endothelial cells. Loss of telomere integrity is a major trigger for the onset of premature aging under mild chronic oxidative stress. The telomeres contain condensed DNA material, giving stability to the chromosomes.[39]
Glutathione is formed in the body from three amino acids (cysteine, glycine, and glutamic acid), and forms a part of the antioxidant enzyme glutathione peroxidase. Undenatured whey protein concentrate (WPC), which is rich in cysteine, raises glutathione levels. Many natural compounds and herbs either enhance glutathione production or spare the breakdown of glutathione, enabling it to recycle and inhibit the oxidation of glutathione.
A family of compounds called isothiocyanates, including 2-phenethyl isothiocyanate and sulforaphane (SFN) derived from cruciferous vegetables such as broccoli sprouts, activate glutathione, reduce oxidative damage, and aid in detoxification of environmental carcinogens and toxicants. Isothiocyanates act via cytoplasmic Nrf2 to enhance the production of redox-antioxidants throughout the body through the glutathione pathway.[40],[41]
A recent meta-analysis and systematic review of SFN on lipid reduction and weight control assessed mice and rats fed a high-fat diet. SFN supplements decreased the level of body weight and significantly improved lipid profiles in rodents.
Forest plot showing effects of SFN on serum total cholesterol
Forest plot showing effects of SFN on serum low-density lipoprotein cholesterol[42]
Selenium (Se) is an integral part of the enzyme glutathione, one of the central players of the heart’s redox-antioxidant system, and a deficiency is implicated in certain types of heart disease. Myocardial oxidative stress in chronic heart failure may be augmented at least in part by concomitant glutathione deficiency, and the administration of Se could rescue the exhaustion of this selenoprotein, resulting in improved left ventricular function.[43]
“Science without religion is lame, religion without science is blind.”
- Albert Einstein
The Mediterranean Diet as an Alternative to Statins
Statins are not the only anti-atherosclerosis treatments available. Many studies have demonstrated that the Mediterranean diet offers significant protection from heart disease and cancer, and substantially increases lifespan.Several of these recent studies have shown that eating a Mediterranean diet decreases the absolute risk reduction (ARR) of CAD values more effectively than using statin drugs.[44],[45],[46],[47],[48],[49]
The Mediterranean diet includes locally grown wild vegetables, as well other common vegetables, such as cabbage, leafy and root vegetables, bitter greens (including arugula, radicchio, endive), mushrooms, tomatoes and other fruiting vegetables, grapes and berries, fish, a moderate intake of hard cheeses, grains, and plenty of olive oil.
Greater adherence to the Mediterranean diet is associated with significant reduction in overall mortality, mortality from cardiovascular diseases and stroke, incidence of or mortality from cancer, and incidence of Parkinson’s disease and Alzheimer’s disease and mild cognitive impairment.[50] For those taking statins, reducing simple carbohydrates, eating whole foods, and adherence to a high‐fiber diet have been shown to resolve manifestations of SIM.[51]
A 2020 Cochrane meta-analyses (41 total reports) of randomized clinical trials revealed a beneficial effect of the Mediterranean diet on total CVD incidence.[52]
A 2016 study of more than 20,000 adults found that people who follow a Mediterranean diet are much less likely to develop heart disease,and the researchers estimated that up to 4% of all heart disease cases could be prevented with adherence to a Mediterranean diet.[53]
Another study looked at the risk of heart attack, stroke, and death from cardiovascular causes between people who followed a Mediterranean diet and people who did not. The study, which lasted nearly five years, concluded that the risks were about 30 percent lower in people who followed a Mediterranean diet.[54]
If you’re still not convinced that the Mediterranean diet is heart-healthy, check out this 2019 review of studies, which looked at 29 individual studies on the Mediterranean diet. The authors of the review concluded that the Mediterranean diet is protective against various forms of heart disease.[55]
Adopting a Mediterranean diet after a heart attack is almost three times as powerful in reducing mortality as taking a statin. The recently published PREDIMED randomized controlled trial was stopped early after it showed that in high-risk people, the Mediterranean diet achieved a 30% improvement over a “low fat” diet in terms of cardiovascular events.[56]
Lastly, exercise is an effective therapy to prevent metabolic and cardiovascular diseases and may also help to mitigate SIM.[57]
God embraces you as you are—shadow and light, everything. God embraces it, by grace. —Brother David Steindl-Rast
The Importance of Attitude in Health
In the management of health and the prevention of disease, our focus tends to be on drugs (from a conventional perspective) or foods and supplements (from a more natural, health supportive perspective). While I am a strong proponent of a healthy diet and botanical and nutritional supplements, I also believe that we cannot achieve optimal health without attention to attitude.
When one the last time your health-care practitioner talked with you about attitude and health? Did you know that optimism is associated with a significant reduction in cardiovascular events and all-cause mortality according to a systematic review and meta-analysis?
[1] Gregory A. Roth George A. MensahCatherine O. Johnson, Giovanni Addolorato, Enrico Ammirati, Larry M. Baddour, Noël C. Barengo, Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study, J Am Coll Cardiol. 2020 Dec, 76 (25) 2982–3021, https://www.jacc.org/doi/pdf/10.1016/j.jacc.2020.11.010
[2] Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ. 2010 May 20;340:c2197. doi: 10.1136/bmj.c2197.
[3] Phillips PS, Haas RH.Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2003 Jun 17;138(12):1008-9. Scripps Mercy Hospital; San Diego, CA 92103
[4] Jamil S, Iqbal P. Rhabdomyolysis induced by a single dose of a statin. Heart. 2004 Jan;90(1):e3. Medical Directorate, Chesterfield and North Derbyshire Royal Hospital NHS Calow, Chesterfield, UK
[5] Chang JT, Staffa JA, Parks M, Green L. Rhabdomyolysis with HMG-CoA reductase inhibitors and gemfibrozil combination therapy.Pharmacoepidemiol Drug Saf. 2004 Jul;13(7):417-26. Office of Drug Safety, Food and Drug Administration, Rockville, MD 20857, USA. changJ@cder.fda.gov
[6] Bellosta S, Paoletti R, Corsini A. Safety of statins: focus on clinical pharmacokinetics and drug interactions. Circulation. 2004 Jun 15;109(23 Suppl 1):III50-7., Department of Pharmacological Sciences, University of Milan, Milan, Italy.
[7] Langsjoen PH, Langsjoen JO, Langsjoen AM, Lucas LA. Treatment of statin adverse effects with supplemental Coenzyme Q10 and statin drug discontinuation. Biofactors. 2005;25(1-4):147-52.
[8] Stroes E.S., Thompson P.D., Corsini A., Vladutiu G.D., Raal F.J., Ray K.K., Roden M., Stein E., Tokgözoğlu L., Nordestgaard B.G., et al. Statin-associated muscle symptoms: Impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur. Heart J. 2015;36:1012–1022. doi: 10.1093/eurheartj/ehv043
[9] Ahmadi Y, Ghorbanihaghjo A, Naghi-Zadeh M, Yagin NL. Oxidative stress as a possible mechanism of statin-induced myopathy. Inflammopharmacology. 2018 Jun;26(3):667-674. doi: 10.1007/s10787-018-0469-x. Epub 2018 Mar 24. PMID: 29574631.
[10] Bouitbir J, Sanvee GM, Panajatovic MV, Singh F, Krähenbühl S. Mechanisms of statin-associated skeletal muscle-associated symptoms. Pharmacol Res. 2020 Apr;154:104201. doi: 10.1016/j.phrs.2019.03.010. Epub 2019 Mar 12. PMID: 30877064.
[11] Bouitbir J, Singh F, Charles AL, Schlagowski AI, Bonifacio A, Echaniz-Laguna A, Geny B, Krähenbühl S, Zoll J. Statins Trigger Mitochondrial Reactive Oxygen Species-Induced Apoptosis in Glycolytic Skeletal Muscle. Antioxid Redox Signal. 2016 Jan 10;24(2):84-98. doi: 10.1089/ars.2014.6190. PMID: 26414931.
[12] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36.
[13] Schirris TJ, Renkema GH, Ritschel T, Voermans NC, Bilos A, van Engelen BG, Brandt U, Koopman WJ, Beyrath JD, Rodenburg RJ, Willems PH, Smeitink JA, Russel FG. Statin‐induced myopathy is associated with mitochondrial complex III inhibition. Cell Metab 2015;22:399–407
[14] Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D, Alehagen U, Steurer G, Littarru GP; Q-SYMBIO Study Investigators. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014 Dec;2(6):641-9. doi: 10.1016/j.jchf.2014.06.008. Epub 2014 Oct 1. PMID: 25282031.
Azhar, G., Wei, J.Y. New Approaches to Treating Cardiac Cachexia in the Older Patient. Curr Cardiovasc Risk Rep 7, 480–484 (2013). https://doi.org/10.1007/s12170-013-0353-6
[16] Kwak HB, Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014 Sep; 4(2):71-9.
[17] Wolfram Steinborn and Stefan D. Anker, Cardiac Cachexia: Pathophysiology and Clinical Implications, Basic Appl Myol 13 (4): 191-201, 2003
[18] Packer M: The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol 1992; 20: 248-254.
[19] Obisesan TO, Toth MJ, Donaldson K, Gottlieb SS, Fisher ML, Vaitekevicius P, Poehlman ET: Energy expenditure and symptom severity in men with heart failure. Am J Cardiol 1996; 77: 1250-1252.
[20] Durhuus JA, Hansson S, Morville T, Kuhlman AB, Dohlmann TL, Larsen S, Helge JW, Angleys M, Muniesa-Vargas A, Bundgaard JR, Hickson ID, Dela F, Desler C, Rasmussen LJ. Simvastatin improves mitochondrial respiration in peripheral blood cells. Sci Rep. 2020 Oct 12;10(1):17012. doi: 10.1038/s41598-020-73896-2. PMID: 33046789; PMCID: PMC7550337.
[21] Nakayama A, Morita H, Kawahara T, Itoh H, Komuro I. Association between testosterone and lipid profiles under statin therapy and its clinical impact on the cardiovascular event risk. Heart Vessels. 2021 May 26. doi: 10.1007/s00380-021-01872-5. Epub ahead of print. PMID: 34036416.
[22] Hsieh CJ, Huang B. Rosuvastatin decreases testosterone levels but not sexual function in men with type 2 diabetes. Diabetes Res Clin Pract. 2016 Oct;120:81-8. doi: 10.1016/j.diabres.2016.07.026. Epub 2016 Aug 6. PMID: 27525363.
[23] Baspınar O, Bayram F, Korkmaz S, Aksu M, Kocer D, Dizdar OS, Simsek Y, Toth PP. The effects of statin treatment on adrenal and sexual function and nitric oxide levels in hypercholesterolemic male patients treated with a statin. J Clin Lipidol. 2016 Nov-Dec;10(6):1452-1461. doi: 10.1016/j.jacl.2016.09.004. Epub 2016 Sep 13. PMID: 27919363.
[24] Bolat MS, Bakırtaş M, Fırat F, Akdeniz E, Çınar Ö, Erdemir F. The effect of atorvastatin on penile intracavernosal pressure and cavernosal morphology in normocholesterolemic rats. Turk J Urol. 2018 Aug 31;45(2):91-96. doi: 10.5152/tud.2018.98048. PMID: 30183612; PMCID: PMC6368041.
[25] Mollazadeh H, Tavana E, Fanni G, Bo S, Banach M, Pirro M, von Haehling S, Jamialahmadi T, Sahebkar A. Effects of statins on mitochondrial pathways. J Cachexia Sarcopenia Muscle. 2021 Apr;12(2):237-251. doi: 10.1002/jcsm.12654. Epub 2021 Jan 29. PMID: 33511728; PMCID: PMC8061391.
[26] Bilianou E, Carmena R, Ceška R, Corsini A, Erbel R, Flynn PD, Garcia-Moll X, Gumprecht J, Ishibashi S, Jambart S, Kastelein JJ, Maher V, da Silva PM, Masana L, Odawara M, Pedersen TR, Rotella CM, Salti I, Teramoto T, Tokgozoglu L, Toth PP, Valensi P, Vergès B. The use of statins in people at risk of developing diabetes mellitus: evidence and guidance for clinical practice. Atheroscler Suppl. 2014 Jun;15(1):1-15. doi: 10.1016/j.atherosclerosissup.2014.04.001. PMID: 24840509.
[27] Maki KC, Diwadkar-Navsariwala V, Kramer MW. Statin use and risk for type 2 diabetes: what clinicians should know. Postgrad Med. 2018 Mar;130(2):166-172. doi: 10.1080/00325481.2018.1402658. Epub 2017 Nov 22. PMID: 29139315. Sattar NA, Ginsberg H, Ray K, Chapman MJ, Arca M, Averna M, Betteridge DJ, Bhatnagar D,
[28] Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 2002;360:1623–1630.
[29] Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, et al. Statins and risk of incident diabetes: a collaborative meta‐analysis of randomised statin trials. Lancet 2010;375:735–742.
[30] King DS, Wilburn AJ, Wofford MR, Harrell TK, Lindley BJ, Jones DW. Cognitive impairment associated with atorvastatin and simvastatin. Pharmacotherapy. 2003 Dec;23(12):1663-7.
[31] Muldoon MF, Ryan CM, Sereika SM, Flory JD, Manuck SB. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am J Med. 2004 Dec 1;117(11):823-9.
[32] Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy. 2003 Jul;23(7):871-80.
[33] Christopher-Stine L, Basharat P. Statin-associated immune-mediated myopathy: biology and clinical implications. Curr Opin Lipidol. 2017 Apr;28(2):186-192. doi: 10.1097/MOL.0000000000000399. PMID: 28207435
[34] Lakatta, E. G. and Levy, D. (2003). Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation107, 139-146
[35] Kaplan RC, Frishman WH, Systemic inflammation as a cardiovascular disease risk factor and as a potential target for drug therapy. Heart Dis 2001 Sep-Oct;3(5):326-32.
[36] Haruki Shimizu, Yutaka Kiyohara, Isao Kato, Takanari Kitazono, Yumihiro Tanizaki, Michiaki Kubo, Hirofumi Ueno, Setsuro Ibayashi, Masatoshi Fujishima, and Mitsuo Iida, Relationship Between Plasma Glutathione Levels and Cardiovascular Disease in a Defined Population: The Hisayama Study, Stroke, Sep 2004; 35: 2072 – 2077.
[37] Campolo J, De Maria R, Caruso R, Accinni R, Turazza F, Parolini M, Roubina E, De Chiara B, Cighetti G, Frigerio M, Vitali E, Parodi O. Blood glutathione as independent marker of lipid peroxidation in heart failure. Int J Cardiol. 2007 Apr 12;117(1):45-50. Epub 2006 Aug 1
[38] Campolo J, Caruso R, De Maria R, Parolini M, Oliva F, Roubina E, Cighetti G, Frigerio M, Vitali E, Parodi O. Aminothiol redox alterations in patients with chronic heart failure of ischaemic or non-ischaemic origin. J Cardiovasc Med (Hagerstown). 2007 Dec;8(12):1024-1028.
[39] David J. Kurz1, Stephanie Decary, Ying Hong, Elisabeth Trivier, Alexander Akhmedov, Jorge D. Erusalimsky, Chronic oxidative stress compromises telomere integrity and accelerates the onset of senescence in human endothelial cells, Accepted 9 January 2004, Journal of Cell Science 117, 2417-2426
[40] Yuan JM, Murphy SE, Stepanov I, Wang R, Carmella SG, Nelson HH, Hatsukami D, Hecht SS. 2-Phenethyl Isothiocyanate, Glutathione S-transferase M1 and T1 Polymorphisms, and Detoxification of Volatile Organic Carcinogens and Toxicants in Tobacco Smoke. Cancer Prev Res (Phila). 2016 Jul;9(7):598-606. doi: 10.1158/1940-6207.CAPR-16-0032. Epub 2016 Apr 20. PMID: 27099270; PMCID: PMC4930697.
[41] Ladak Z, Garcia E, Yoon J, Landry T, Armstrong EA, Yager JY, Persad S. Sulforaphane (SFA) protects neuronal cells from oxygen & glucose deprivation (OGD). PLoS One. 2021 Mar 18;16(3):e0248777. doi: 10.1371/journal.pone.0248777. PMID: 33735260; PMCID: PMC7971874.
[42] Du K, Fan Y, Li D. Sulforaphane ameliorates lipid profile in rodents: an updated systematic review and meta-analysis. Sci Rep. 2021 Apr 8;11(1):7804. doi: 10.1038/s41598-021-87367-9. PMID: 33833347; PMCID: PMC8032686.
[43] Hiraoka Y. Association between function of selenium and heart disease, Nihon Rinsho. 2016 Jul;74(7):1192-8.
[44] Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA.Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004 Sep 22;292(12):1433-9.
[45] de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994 Jun 11;343(8911):1454-9. Erratum in: Lancet 1995 Mar 18;345(8951):738.
[46] de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999 Feb 16;99(6):779-85.
[47] Trichopoulou A, Bamia C, Trichopoulos D. Mediterranean diet and survival among patients with coronary heart disease in Greece. Arch Intern Med. 2005 Apr 25;165(8):929-35.
[48] Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, Manor O, Pella D, Berry EM. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002 Nov 9;360(9344):1455-61.
[49] de Lorgeril M, Salen P, Martin JL, Monjaud I, Boucher P, Mamelle N. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998 Jun 8;158(11):1181-7.
[50] Demarin V, Lisak M, Morović S. Mediterranean diet in healthy lifestyle and prevention of stroke. Acta Clin Croat. 2011 Mar;50(1):67-77.
[51] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36
[52] Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, Rahelić D, Sievenpiper JL, Salas-Salvadó J. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. 2020;60(7):1207-1227. doi: 10.1080/10408398.2019.1565281. Epub 2019 Jan 24. PMID: 30676058.
[53] Tong, T.Y.N., Wareham, N.J., Khaw, K. et al. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study. BMC Med 14, 135, (2016). https://doi.org/10.1186/s12916-016-0677-4
[54] Bailén Almorox R. Prevención primaria de la enfermedad cardiovascular con una dieta mediterránea [Cardiovascular disease primary prevention with a Mediterranean diet]. Rev Clin Esp (Barc). 2013 Oct;213(7):355-6. Spanish. doi: 10.1016/j.rce.2013.04.011. PMID: 24244956.
[55] Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173–191. doi:10.1007/s00394-017-1582-0.
[56] Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013 Apr 4;368(14):1279-90. doi: 10.1056/NEJMoa1200303. Epub 2013 Feb 25.
[57] Kwak HB. Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014;4(2):71-79. doi:10.15280/jlm.2014.4.2.71
[58] Alan Rozanski, MD; Chirag Bavishi, MD, MPH; Laura D. Kubzansky, PhD; Randy Cohen, MD, Association of Optimism With Cardiovascular Events and All-Cause Mortality A Systematic Review and Meta-analysis, JAMA Network Open. 2019;2(9):e1912200. doi:10.1001/jamanetworkopen.2019.12200
For some people, statin drugs do more harm than good. In a study that examined data from over two million patients, including over 225,000 patients who were new statin drug users, researchers found that for every 10,000 women treated with statins, there were only 271 fewer cases of heart disease. At the same time, the statins caused 74 cases of liver damage, 23 cases of acute kidney failure, 39 cases of extreme muscle weakness and 307 cases of cataracts. Statin drugs, in other words, helped 271 people but harmed 443 people. This demonstrates how statins are wreaking havoc with the health of those who take them causing damage that far outweighs any benefit they might offer.[2]
Statins are the most widely used drugs for treating hyperlipidemia. Although these drugs are purported to be safe, many patients taking them suffer from myopathy (muscle weakness). [3],[4],[5],[6],[7] This is concerning, because the heart is a muscle that never stops working in its job of pumping blood throughout the body. Statin-associated muscular symptoms range from asymptomatic elevation of serum creatine kinase (CK) to life-threatening rhabdomyolysis.[8] Several molecular mechanisms underlie statin-induced myopathy, including a decrease in levels of essential mevalonate and cholesterol derivatives.[9]
Skeletal muscle-associated symptoms (SAMS) are a frequent reason for stopping treatment with statins. Common SAMS include fatigue, weakness and pain, possibly accompanied by elevated serum creatine kinase activity. The most severe muscular adverse reaction is the potentially fatal rhabdomyolysis, which is whole-scale muscle breakdown. In most cases, rhabdomyolysis occurs following the use of these drugs for at least one week. But cases of rhabdomyolysis after just a single dose of simvastatin have been reported.44
The frequency of SAMS is variable but occurs in up to 30% of patients taking statins.[10]
The Effect of Statins on COQ-10 Levels and Mitochondria
Mitochondria are the tiny “engines” of our cells. Studies show that statins have several negative effects on mitochondria, including reduction of coenzyme Q10 levels, inhibition of respiratory chain complexes, induction of mitochondrial apoptosis, and dysregulation of Ca2+ metabolism and carnitine palmitoyltransferase-2 expression.
Treatment with statin drugs is associated with mitochondrial oxidative stress, which activates apoptosis and contributes to myopathy. Glycolytic muscles are more sensitive to atorvastatin than oxidative muscles, likely because of the higher antioxidative capacity in oxidative muscles.[11] Statin-induced myopathy (SIM) is a secondary mitochondrial myopathy,[12] since statins exhibit their side effects mainly by interaction with mitochondria.[13]
A deficiency of CoQ10 has been linked to congestive heart failure (CHF), which is a leading cause of morbidity and mortality in the elderly and accounts for more hospitalizations than any other condition. A 2-year, multicenter study of 420 patients with moderate to severe CHF showed that adding CoQ10 (100 mg three times daily) to conventional drug therapy reduced CV mortality by 42% and all-cause mortality by 44%. It also reduced CHF-related hospitalizations.[14]
Advanced stages of CHF can be associated with serious complications such as cardiac cachexia (defined as unintentional weight loss of more than 6 % in 6 months). Cardiac cachexia and the associated progressive weight loss are sometimes overlooked by older patients, their families and care providers.[15] Statins also reduce exercise capacity, and long-term use can lead to decreased skeletal muscle strength and increased risk of falling in elderly patients.[16]
Statin-related side effects, including statin cardiomyopathy, are far more common than previously recognized. However, these side effects are reversible with the combination of statin discontinuation and supplemental CoQ10 and other mitochondrial-enhancing nutrients and botanicals.Ubiquinol, the reduced form of CoQ10, has significantly higher absorption and bioavailability than non-reduced form (ubiquinone), making it the best choice for people with chronic inflammation or an inflamed digestive tract.
Neuroendocrine and Endocrine Abnormalities are a Major Contributor to Cardiac Cachexia and Statin-Induced Myopathy (SIM)
Impaired cardiac function is linked to general neurohormonal activation via stimulation of the sympathetic nervous system, the renin-angiotensin-aldosterone axis and the natriuretic peptide system. At the onset of cardiac heart failure, these systems are thought to be beneficial, but they contribute to increased vascular resistance and afterload, ventricular enlargement, and remodeling. The neurohormonal hypothesis postulates that heart failure progresses as a result of activation of endogenous neurohormonal systems, which exert deleterious effects on the heart and circulation.[17]
Research shows that the stress hormone cortisol is part of the general stress response with a catabolic action increased manifestly (2.5-fold) in untreated CHF patients with severe disease and particularly in cachectic CHF patients.[18] The clinical severity of CHF illness corresponds to the degree of the increase in resting energy demands. Plasma norepinephrine may reflect overall sympathetic activity.[19]
Statin drugs, such as Simvastatin induce myotube atrophy and cell loss that is associated with impaired ADP-stimulated maximal mitochondrial respiratory capacity, mitochondrial oxidative stress, and apoptosis in primary human skeletal myotubes, suggesting that mitochondrial dysfunction may underlie human statin-induced myopathy. SIM suggests a correlation with impairment of mitochondrial function. Long-term treatment with statin drugs increases respiration and the production of superoxide in mitochondria of peripheral blood mononuclear cells (PBMCs) and platelets.[20]
Along with lowering low-density lipoprotein cholesterol (LDL-C) levels, statin therapy can decrease the levels of serum steroid hormones, including testosterone and cortisol. [21],[22] Low testosterone in men is a major risk factor for cardiovascular disease and has other deleterious effects, including erectile dysfunction.[23],[24] Adding to the problem is that many men aromatize (convert) their testosterone into estrogen, and elevated estrogen in men is a cardiovascular risk factor as well. Yet, treating men with testosterone not only does not help, it appears to increase this risk.
Instead of prescribing hormones, my philosophy is to restore Essence, which is the reservoir from which we create hormones. This is accomplished through dietary and lifestyle support, as well as through the use of specific herbs that nourish and restore vitality.
Additional Risks of Statin Use: Diabetes, Cognitive Decline, and Dementia
In addition to muscular and cardiovascular risks, the use of statins has been associated with the onset of pathological conditions like diabetes and dementia. This is a result of interference with mitochondrial pathways by various mechanisms, such as reduction in mitochondrial oxidative phosphorylation, increase in oxidative stress, decrease in uncoupling protein 3 concentration, and interference in amyloid-β metabolism.[25]
The US Food and Drug Administration (FDA) now requires labeling requirements for statins to include a warning about the possibility of increased blood sugar and HbA1c levels and the European Medicines Agency to issue guidance on a small increased risk of T2D with the statin class.[26]
In recent years, several randomized, controlled trials and observational studies have reported increased risk for new-onset type 2 diabetes mellitus (T2D) with statin treatment, particularly with use of high-intensity statins that reduce LDL-C by 50% or more.[27].[28],[29]
Taking statin drugs also appears to reduce cognitive function. Researchers in the journal Pharmacotherapy reported two women who experienced significant cognitive impairment temporally related to statin therapy. One woman took Atorvastatin, and the other first took Atorvastatin, then was rechallenged with Simvastatin. The researchers warned that clinicians should be aware of cognitive impairment and dementia as potential adverse effects associated with statin therapy.[30]
A larger study observed 283 people—94 in the placebo group, 96 in the 10-mg Simvastatin group, and 93 in the 40-mg Simvastatin group. Compared with the placebo, Simvastatin was associated with minor negative changes in performance on several tests assessing attention, memory, and overall mental efficiency. In the team’s earlier trial, 20 mg of Lovastatin given every day for six months produced similar changes on the same tests.[31]
A survey by the MedWatch drug surveillance system of the Food and Drug Administration (FDA) from November 1997-February 2002 for reports of statin-associated memory loss identified 60 patients who had memory loss associated with statins. About 50% of the patients noted cognitive adverse effects within 2 months of therapy. Fourteen (56%) of 25 patients noted improvement when the statin was discontinued. There are no available prospective studies that show cognitive or anti-amyloid benefits for any statin, although some people are actually touting statins to be beneficial for the prevention of dementia.[32]
Statin-Related Autoimmune Myopathy
Recently, our understanding of statin-associated myopathy has expanded to include not only a toxic myopathy with limited and reversible side-effects but also an autoimmune variety. In this case, statins likely induce an autoimmune myopathy that is both associated with a specific autoantibody and is responsive to immunosuppression and immune modulation.
Statin-associated immune-mediated myopathy provides an example of an environmental trigger (statins) directly implicated in an autoimmune disease associated with a genetic predisposition as well as potential risk factors including concomitant diseases and specific statins.[33]
What Really Causes Vascular Disease?
Diseases of the vascular system have long been considered to be age-related in terms of their onset and progression.[34] Although there is a small amount of truth with regard to the role lipid balance plays in health as one ages, it is no more important than oxidative damage and glutathione-dependent redox homeostasis. Cardiovascular disease is most often caused by a chain of effects that increase catabolic activity while decreasing anabolic activity. This includes hormone dysfunction/imbalance (loss of testosterone, DHEA, growth hormone, or elevated cortisol and/or insulin), key receptors and enzymes, pro-inflammatory and oxidative damage, elevated fibrinogen, and mitochondrial atrophy.
Atherosclerosis, the main cause of cardiovascular disease, is a chronic inflammatory condition[35] that associated with an overproduction of oxidant species, namely peroxynitrite, which is a powerful oxidant that reacts directly with all biomolecules. Glutathione is an efficient scavenger of peroxynitrite, so, modulation of glutathione synthesis may provide a strategy to selectively protect cells from this oxidant. Higher levels of plasma glutathione are associated with a lower incidence of cardiovascular disease.[36]
Abnormalities in intracellular GSH cycling are associated with increased lipid peroxidation in congestive heart failure.[37] Also, reduced sulfur-containing amino acid alterations have been found in the progression of chronic ischemic heart disease to heart failure status, as an additional pro-oxidant stimulus for worsening oxidative stress.[38]
A key role for glutathione-dependent redox homeostasis is the preservation of telomere function in endothelial cells. Loss of telomere integrity is a major trigger for the onset of premature aging under mild chronic oxidative stress. The telomeres contain condensed DNA material, giving stability to the chromosomes.[39]
Glutathione is formed in the body from three amino acids (cysteine, glycine, and glutamic acid), and forms a part of the antioxidant enzyme glutathione peroxidase. Undenatured whey protein concentrate (WPC), which is rich in cysteine, raises glutathione levels. Many natural compounds and herbs either enhance glutathione production or spare the breakdown of glutathione, enabling it to recycle and inhibit the oxidation of glutathione.
A family of compounds called isothiocyanates, including 2-phenethyl isothiocyanate and sulforaphane (SFN) derived from cruciferous vegetables such as broccoli sprouts, activate glutathione, reduce oxidative damage, and aid in detoxification of environmental carcinogens and toxicants. Isothiocyanates act via cytoplasmic Nrf2 to enhance the production of redox-antioxidants throughout the body through the glutathione pathway.[40],[41]
A recent meta-analysis and systematic review of SFN on lipid reduction and weight control assessed mice and rats fed a high-fat diet. SFN supplements decreased the level of body weight and significantly improved lipid profiles in rodents.
Forest plot showing effects of SFN on serum total cholesterol
Forest plot showing effects of SFN on serum low-density lipoprotein cholesterol[42]
Selenium (Se) is an integral part of the enzyme glutathione, one of the central players of the heart’s redox-antioxidant system, and a deficiency is implicated in certain types of heart disease. Myocardial oxidative stress in chronic heart failure may be augmented at least in part by concomitant glutathione deficiency, and the administration of Se could rescue the exhaustion of this selenoprotein, resulting in improved left ventricular function.[43]
“Science without religion is lame, religion without science is blind.”
- Albert Einstein
The Mediterranean Diet as an Alternative to Statins
Statins are not the only anti-atherosclerosis treatments available. Many studies have demonstrated that the Mediterranean diet offers significant protection from heart disease and cancer, and substantially increases lifespan.Several of these recent studies have shown that eating a Mediterranean diet decreases the absolute risk reduction (ARR) of CAD values more effectively than using statin drugs.[44],[45],[46],[47],[48],[49]
The Mediterranean diet includes locally grown wild vegetables, as well other common vegetables, such as cabbage, leafy and root vegetables, bitter greens (including arugula, radicchio, endive), mushrooms, tomatoes and other fruiting vegetables, grapes and berries, fish, a moderate intake of hard cheeses, grains, and plenty of olive oil.
Greater adherence to the Mediterranean diet is associated with significant reduction in overall mortality, mortality from cardiovascular diseases and stroke, incidence of or mortality from cancer, and incidence of Parkinson’s disease and Alzheimer’s disease and mild cognitive impairment.[50] For those taking statins, reducing simple carbohydrates, eating whole foods, and adherence to a high‐fiber diet have been shown to resolve manifestations of SIM.[51]
A 2020 Cochrane meta-analyses (41 total reports) of randomized clinical trials revealed a beneficial effect of the Mediterranean diet on total CVD incidence.[52]
A 2016 study of more than 20,000 adults found that people who follow a Mediterranean diet are much less likely to develop heart disease,and the researchers estimated that up to 4% of all heart disease cases could be prevented with adherence to a Mediterranean diet.[53]
Another study looked at the risk of heart attack, stroke, and death from cardiovascular causes between people who followed a Mediterranean diet and people who did not. The study, which lasted nearly five years, concluded that the risks were about 30 percent lower in people who followed a Mediterranean diet.[54]
If you’re still not convinced that the Mediterranean diet is heart-healthy, check out this 2019 review of studies, which looked at 29 individual studies on the Mediterranean diet. The authors of the review concluded that the Mediterranean diet is protective against various forms of heart disease.[55]
Adopting a Mediterranean diet after a heart attack is almost three times as powerful in reducing mortality as taking a statin. The recently published PREDIMED randomized controlled trial was stopped early after it showed that in high-risk people, the Mediterranean diet achieved a 30% improvement over a “low fat” diet in terms of cardiovascular events.[56]
Lastly, exercise is an effective therapy to prevent metabolic and cardiovascular diseases and may also help to mitigate SIM.[57]
God embraces you as you are—shadow and light, everything. God embraces it, by grace. —Brother David Steindl-Rast
The Importance of Attitude in Health
In the management of health and the prevention of disease, our focus tends to be on drugs (from a conventional perspective) or foods and supplements (from a more natural, health supportive perspective). While I am a strong proponent of a healthy diet and botanical and nutritional supplements, I also believe that we cannot achieve optimal health without attention to attitude.
When one the last time your health-care practitioner talked with you about attitude and health? Did you know that optimism is associated with a significant reduction in cardiovascular events and all-cause mortality according to a systematic review and meta-analysis?
[1] Gregory A. Roth George A. MensahCatherine O. Johnson, Giovanni Addolorato, Enrico Ammirati, Larry M. Baddour, Noël C. Barengo, Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study, J Am Coll Cardiol. 2020 Dec, 76 (25) 2982–3021, https://www.jacc.org/doi/pdf/10.1016/j.jacc.2020.11.010
[2] Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ. 2010 May 20;340:c2197. doi: 10.1136/bmj.c2197.
[3] Phillips PS, Haas RH.Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2003 Jun 17;138(12):1008-9. Scripps Mercy Hospital; San Diego, CA 92103
[4] Jamil S, Iqbal P. Rhabdomyolysis induced by a single dose of a statin. Heart. 2004 Jan;90(1):e3. Medical Directorate, Chesterfield and North Derbyshire Royal Hospital NHS Calow, Chesterfield, UK
[5] Chang JT, Staffa JA, Parks M, Green L. Rhabdomyolysis with HMG-CoA reductase inhibitors and gemfibrozil combination therapy.Pharmacoepidemiol Drug Saf. 2004 Jul;13(7):417-26. Office of Drug Safety, Food and Drug Administration, Rockville, MD 20857, USA. changJ@cder.fda.gov
[6] Bellosta S, Paoletti R, Corsini A. Safety of statins: focus on clinical pharmacokinetics and drug interactions. Circulation. 2004 Jun 15;109(23 Suppl 1):III50-7., Department of Pharmacological Sciences, University of Milan, Milan, Italy.
[7] Langsjoen PH, Langsjoen JO, Langsjoen AM, Lucas LA. Treatment of statin adverse effects with supplemental Coenzyme Q10 and statin drug discontinuation. Biofactors. 2005;25(1-4):147-52.
[8] Stroes E.S., Thompson P.D., Corsini A., Vladutiu G.D., Raal F.J., Ray K.K., Roden M., Stein E., Tokgözoğlu L., Nordestgaard B.G., et al. Statin-associated muscle symptoms: Impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur. Heart J. 2015;36:1012–1022. doi: 10.1093/eurheartj/ehv043
[9] Ahmadi Y, Ghorbanihaghjo A, Naghi-Zadeh M, Yagin NL. Oxidative stress as a possible mechanism of statin-induced myopathy. Inflammopharmacology. 2018 Jun;26(3):667-674. doi: 10.1007/s10787-018-0469-x. Epub 2018 Mar 24. PMID: 29574631.
[10] Bouitbir J, Sanvee GM, Panajatovic MV, Singh F, Krähenbühl S. Mechanisms of statin-associated skeletal muscle-associated symptoms. Pharmacol Res. 2020 Apr;154:104201. doi: 10.1016/j.phrs.2019.03.010. Epub 2019 Mar 12. PMID: 30877064.
[11] Bouitbir J, Singh F, Charles AL, Schlagowski AI, Bonifacio A, Echaniz-Laguna A, Geny B, Krähenbühl S, Zoll J. Statins Trigger Mitochondrial Reactive Oxygen Species-Induced Apoptosis in Glycolytic Skeletal Muscle. Antioxid Redox Signal. 2016 Jan 10;24(2):84-98. doi: 10.1089/ars.2014.6190. PMID: 26414931.
[12] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36.
[13] Schirris TJ, Renkema GH, Ritschel T, Voermans NC, Bilos A, van Engelen BG, Brandt U, Koopman WJ, Beyrath JD, Rodenburg RJ, Willems PH, Smeitink JA, Russel FG. Statin‐induced myopathy is associated with mitochondrial complex III inhibition. Cell Metab 2015;22:399–407
[14] Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D, Alehagen U, Steurer G, Littarru GP; Q-SYMBIO Study Investigators. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014 Dec;2(6):641-9. doi: 10.1016/j.jchf.2014.06.008. Epub 2014 Oct 1. PMID: 25282031.
Azhar, G., Wei, J.Y. New Approaches to Treating Cardiac Cachexia in the Older Patient. Curr Cardiovasc Risk Rep 7, 480–484 (2013). https://doi.org/10.1007/s12170-013-0353-6
[16] Kwak HB, Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014 Sep; 4(2):71-9.
[17] Wolfram Steinborn and Stefan D. Anker, Cardiac Cachexia: Pathophysiology and Clinical Implications, Basic Appl Myol 13 (4): 191-201, 2003
[18] Packer M: The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol 1992; 20: 248-254.
[19] Obisesan TO, Toth MJ, Donaldson K, Gottlieb SS, Fisher ML, Vaitekevicius P, Poehlman ET: Energy expenditure and symptom severity in men with heart failure. Am J Cardiol 1996; 77: 1250-1252.
[20] Durhuus JA, Hansson S, Morville T, Kuhlman AB, Dohlmann TL, Larsen S, Helge JW, Angleys M, Muniesa-Vargas A, Bundgaard JR, Hickson ID, Dela F, Desler C, Rasmussen LJ. Simvastatin improves mitochondrial respiration in peripheral blood cells. Sci Rep. 2020 Oct 12;10(1):17012. doi: 10.1038/s41598-020-73896-2. PMID: 33046789; PMCID: PMC7550337.
[21] Nakayama A, Morita H, Kawahara T, Itoh H, Komuro I. Association between testosterone and lipid profiles under statin therapy and its clinical impact on the cardiovascular event risk. Heart Vessels. 2021 May 26. doi: 10.1007/s00380-021-01872-5. Epub ahead of print. PMID: 34036416.
[22] Hsieh CJ, Huang B. Rosuvastatin decreases testosterone levels but not sexual function in men with type 2 diabetes. Diabetes Res Clin Pract. 2016 Oct;120:81-8. doi: 10.1016/j.diabres.2016.07.026. Epub 2016 Aug 6. PMID: 27525363.
[23] Baspınar O, Bayram F, Korkmaz S, Aksu M, Kocer D, Dizdar OS, Simsek Y, Toth PP. The effects of statin treatment on adrenal and sexual function and nitric oxide levels in hypercholesterolemic male patients treated with a statin. J Clin Lipidol. 2016 Nov-Dec;10(6):1452-1461. doi: 10.1016/j.jacl.2016.09.004. Epub 2016 Sep 13. PMID: 27919363.
[24] Bolat MS, Bakırtaş M, Fırat F, Akdeniz E, Çınar Ö, Erdemir F. The effect of atorvastatin on penile intracavernosal pressure and cavernosal morphology in normocholesterolemic rats. Turk J Urol. 2018 Aug 31;45(2):91-96. doi: 10.5152/tud.2018.98048. PMID: 30183612; PMCID: PMC6368041.
[25] Mollazadeh H, Tavana E, Fanni G, Bo S, Banach M, Pirro M, von Haehling S, Jamialahmadi T, Sahebkar A. Effects of statins on mitochondrial pathways. J Cachexia Sarcopenia Muscle. 2021 Apr;12(2):237-251. doi: 10.1002/jcsm.12654. Epub 2021 Jan 29. PMID: 33511728; PMCID: PMC8061391.
[26] Bilianou E, Carmena R, Ceška R, Corsini A, Erbel R, Flynn PD, Garcia-Moll X, Gumprecht J, Ishibashi S, Jambart S, Kastelein JJ, Maher V, da Silva PM, Masana L, Odawara M, Pedersen TR, Rotella CM, Salti I, Teramoto T, Tokgozoglu L, Toth PP, Valensi P, Vergès B. The use of statins in people at risk of developing diabetes mellitus: evidence and guidance for clinical practice. Atheroscler Suppl. 2014 Jun;15(1):1-15. doi: 10.1016/j.atherosclerosissup.2014.04.001. PMID: 24840509.
[27] Maki KC, Diwadkar-Navsariwala V, Kramer MW. Statin use and risk for type 2 diabetes: what clinicians should know. Postgrad Med. 2018 Mar;130(2):166-172. doi: 10.1080/00325481.2018.1402658. Epub 2017 Nov 22. PMID: 29139315. Sattar NA, Ginsberg H, Ray K, Chapman MJ, Arca M, Averna M, Betteridge DJ, Bhatnagar D,
[28] Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 2002;360:1623–1630.
[29] Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, et al. Statins and risk of incident diabetes: a collaborative meta‐analysis of randomised statin trials. Lancet 2010;375:735–742.
[30] King DS, Wilburn AJ, Wofford MR, Harrell TK, Lindley BJ, Jones DW. Cognitive impairment associated with atorvastatin and simvastatin. Pharmacotherapy. 2003 Dec;23(12):1663-7.
[31] Muldoon MF, Ryan CM, Sereika SM, Flory JD, Manuck SB. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am J Med. 2004 Dec 1;117(11):823-9.
[32] Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy. 2003 Jul;23(7):871-80.
[33] Christopher-Stine L, Basharat P. Statin-associated immune-mediated myopathy: biology and clinical implications. Curr Opin Lipidol. 2017 Apr;28(2):186-192. doi: 10.1097/MOL.0000000000000399. PMID: 28207435
[34] Lakatta, E. G. and Levy, D. (2003). Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation107, 139-146
[35] Kaplan RC, Frishman WH, Systemic inflammation as a cardiovascular disease risk factor and as a potential target for drug therapy. Heart Dis 2001 Sep-Oct;3(5):326-32.
[36] Haruki Shimizu, Yutaka Kiyohara, Isao Kato, Takanari Kitazono, Yumihiro Tanizaki, Michiaki Kubo, Hirofumi Ueno, Setsuro Ibayashi, Masatoshi Fujishima, and Mitsuo Iida, Relationship Between Plasma Glutathione Levels and Cardiovascular Disease in a Defined Population: The Hisayama Study, Stroke, Sep 2004; 35: 2072 – 2077.
[37] Campolo J, De Maria R, Caruso R, Accinni R, Turazza F, Parolini M, Roubina E, De Chiara B, Cighetti G, Frigerio M, Vitali E, Parodi O. Blood glutathione as independent marker of lipid peroxidation in heart failure. Int J Cardiol. 2007 Apr 12;117(1):45-50. Epub 2006 Aug 1
[38] Campolo J, Caruso R, De Maria R, Parolini M, Oliva F, Roubina E, Cighetti G, Frigerio M, Vitali E, Parodi O. Aminothiol redox alterations in patients with chronic heart failure of ischaemic or non-ischaemic origin. J Cardiovasc Med (Hagerstown). 2007 Dec;8(12):1024-1028.
[39] David J. Kurz1, Stephanie Decary, Ying Hong, Elisabeth Trivier, Alexander Akhmedov, Jorge D. Erusalimsky, Chronic oxidative stress compromises telomere integrity and accelerates the onset of senescence in human endothelial cells, Accepted 9 January 2004, Journal of Cell Science 117, 2417-2426
[40] Yuan JM, Murphy SE, Stepanov I, Wang R, Carmella SG, Nelson HH, Hatsukami D, Hecht SS. 2-Phenethyl Isothiocyanate, Glutathione S-transferase M1 and T1 Polymorphisms, and Detoxification of Volatile Organic Carcinogens and Toxicants in Tobacco Smoke. Cancer Prev Res (Phila). 2016 Jul;9(7):598-606. doi: 10.1158/1940-6207.CAPR-16-0032. Epub 2016 Apr 20. PMID: 27099270; PMCID: PMC4930697.
[41] Ladak Z, Garcia E, Yoon J, Landry T, Armstrong EA, Yager JY, Persad S. Sulforaphane (SFA) protects neuronal cells from oxygen & glucose deprivation (OGD). PLoS One. 2021 Mar 18;16(3):e0248777. doi: 10.1371/journal.pone.0248777. PMID: 33735260; PMCID: PMC7971874.
[42] Du K, Fan Y, Li D. Sulforaphane ameliorates lipid profile in rodents: an updated systematic review and meta-analysis. Sci Rep. 2021 Apr 8;11(1):7804. doi: 10.1038/s41598-021-87367-9. PMID: 33833347; PMCID: PMC8032686.
[43] Hiraoka Y. Association between function of selenium and heart disease, Nihon Rinsho. 2016 Jul;74(7):1192-8.
[44] Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA.Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004 Sep 22;292(12):1433-9.
[45] de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994 Jun 11;343(8911):1454-9. Erratum in: Lancet 1995 Mar 18;345(8951):738.
[46] de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999 Feb 16;99(6):779-85.
[47] Trichopoulou A, Bamia C, Trichopoulos D. Mediterranean diet and survival among patients with coronary heart disease in Greece. Arch Intern Med. 2005 Apr 25;165(8):929-35.
[48] Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, Manor O, Pella D, Berry EM. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002 Nov 9;360(9344):1455-61.
[49] de Lorgeril M, Salen P, Martin JL, Monjaud I, Boucher P, Mamelle N. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998 Jun 8;158(11):1181-7.
[50] Demarin V, Lisak M, Morović S. Mediterranean diet in healthy lifestyle and prevention of stroke. Acta Clin Croat. 2011 Mar;50(1):67-77.
[51] Fitzgerald K, Redmond E, Harbor C. Statin‐induced myopathy. Glob Adv Health Med 2012;1:32–36
[52] Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, Rahelić D, Sievenpiper JL, Salas-Salvadó J. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. 2020;60(7):1207-1227. doi: 10.1080/10408398.2019.1565281. Epub 2019 Jan 24. PMID: 30676058.
[53] Tong, T.Y.N., Wareham, N.J., Khaw, K. et al. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study. BMC Med 14, 135, (2016). https://doi.org/10.1186/s12916-016-0677-4
[54] Bailén Almorox R. Prevención primaria de la enfermedad cardiovascular con una dieta mediterránea [Cardiovascular disease primary prevention with a Mediterranean diet]. Rev Clin Esp (Barc). 2013 Oct;213(7):355-6. Spanish. doi: 10.1016/j.rce.2013.04.011. PMID: 24244956.
[55] Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173–191. doi:10.1007/s00394-017-1582-0.
[56] Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013 Apr 4;368(14):1279-90. doi: 10.1056/NEJMoa1200303. Epub 2013 Feb 25.
[57] Kwak HB. Statin-induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014;4(2):71-79. doi:10.15280/jlm.2014.4.2.71
[58] Alan Rozanski, MD; Chirag Bavishi, MD, MPH; Laura D. Kubzansky, PhD; Randy Cohen, MD, Association of Optimism With Cardiovascular Events and All-Cause Mortality A Systematic Review and Meta-analysis, JAMA Network Open. 2019;2(9):e1912200. doi:10.1001/jamanetworkopen.2019.12200

From the insightful commentary to the captivating writing, every word of this post is top-notch. Kudos to the author for producing such fantastic content.