“Medicine qua medicine comes into existence when it appropriates knowledge and skills, no matter what their origin, in order to further its healing purposes.” — Edmund Pellegrino
The world population is aging with a rapid increase in the very elderly aged 80 and up. Those who make it to 100 and beyond (centenarians) are considered an exceptional human model of healthy aging and extreme longevity.
In general, centenarians appear to escape—or at least significantly delay—the diseases of aging that normally cause mortality at earlier ages. In an attempt to understand why some people live well beyond what is currently considered to be the ‘normal’ lifespan, gerontologists have identified a variety of factors that centenarians share. These include not smoking, a healthy diet, regular exercise, avoidance of stress, family connectedness, and a positive attitude.
Centenarians are characterized by extremely heterogeneous health status and different degree of frailty, compared to a very narrow range of chronological age.[1] Frailty is one of the most devastating effects of aging, and manifests as weakness, weight loss, and low activity. This syndrome of decreased physiological reserves and vulnerability to stressors leads to adverse health outcomes.
An interesting recent finding is that high cholesterol levels are associated with extreme longevity.[2] Cholesterol levels naturally tend to rise with age, and current medical thinking and practice has been to keep cholesterol levels low, primarily through the use of cholesterol-lowering drugs. It’s perhaps time to rethink that approach.
Questioning the Current Cholesterol Guidelines
Despite the current emphasis on achieving low cholesterol levels, the fact is that low cholesterol is not associated with a longer life span. Studies show that high LDL-C is inversely associated with mortality in most people over 60 years. This finding is inconsistent with the cholesterol hypothesis (ie, that cholesterol, particularly LDL-C, is inherently atherogenic). Since elderly people with high LDL-C live as long or longer than those with low LDL-C, there is good reason to question the validity of the cholesterol hypothesis.
Ideally, risk factors should help us distinguish those who will develop a disease from those who will not. However, if one examines the original Framingham Heart Study data (as an example) it is clear that the cholesterol levels of those who developed CHD and those who did not overlap except when the total cholesterol level exceeded 380 mg/dL or was less than 150 mg/dL.[3]
Clearly, association does not equal causation, and it may be a leap of faith to assume that lowering cholesterol is the best way to prevent coronary heart disease (CHD).
“Faith is much better than belief. Belief is when someone else does the thinking.” ― Buckminster Fuller
The role of blood cholesterol levels in CHD are debatable, and the expectation that CHD could be prevented or eliminated by simply reducing cholesterol appears unfounded. On the contrary, we should acknowledge the inconsistencies of the cholesterol theory and recognize the proven benefits of a healthy lifestyle incorporating a Mediterranean diet for preventing CHD.[4]
Cholesterol levels <200 are not associated with a longer life, and most research demonstrates that higher cholesterol levels between 200 and 260 may be the healthiest range. In fact, research shows that cholesterol levels <150 are associated with a shorter lifespan, depression, and cancer. LDL cholesterol between 100 and 160 appears to be the healthiest range, but a lot depends on the type of LDL.
So why this obsession with “lower is better” when it comes to cholesterol? Although high cholesterol levels have long been assumed to be a major cause of atherosclerosis, there is now plenty of evidence to challenge this theory. Why can’t we come to a definitive conclusion with the large body of scientific data that is available? I believe the answer is very simple: the cholesterol-heart disease theory is an easy answer for everyone, including the physician, the patient, the insurance companies and the drug companies. Furthermore, the financial gain that drug companies realize from cholesterol lowering drugs is significant.
The Dangers of Low Cholesterol Levels
Studies from around the world consistently show that low levels of LDL-C concentration are strongly and independently associated with increased risk of cancer, CVD, and all-cause mortality.
In a Japanese study of 347, 971 subjects, researchers tested the association between low-density lipoprotein cholesterol (LDL-C) and cardiovascular disease (CVD), cancer, and all-cause mortality in non-statin users. Five groups were defined according to baseline LDL-C concentration (<70, 70-99, 100-129, 130-159, ≥160 mg/dL). The lowest LDL-C group (LDL < 70 mg/dL) had a higher risk of all-cause mortality, CVD mortality, and cancer mortality compared to the reference group.
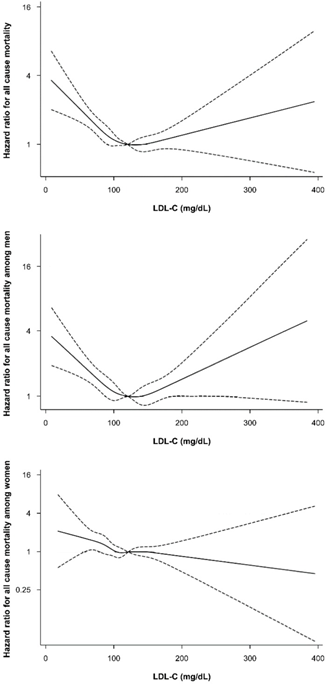
(LDL 120-139 mg/dL).
Spline plot of plasma low-density lipoprotein cholesterol and all-cause mortality rate, normalized to the mortality rate at low-density lipoprotein cholesterol of 100–129 mg/dL. The adjusted hazard ratios and 95% confidence intervals were calculated with Cox proportional-hazards models after adjusting for adjusted for age, BMI, smoking status, alcohol intake, regular exercise, education, income, marital status, diabetes, hypertension, and high-density lipoprotein cholesterol.[5]
In a Danish study published in 2019, researchers set out to determine the association between levels of low-density lipoprotein cholesterol (LDL-C) and all-cause mortality, and the concentration of LDL-C associated with the lowest risk of all-cause mortality in the general population.
Among 108,243 individuals aged 20-100, 11,376 (10.5%) died during the study, at a median age of 81. The association between levels of LDL-C and the risk of all-cause mortality was U shaped, with low and high levels associated with an increased risk of all-cause mortality.
Compared with individuals with concentrations of LDL-C of 132-154 mg/dL, the multivariable adjusted hazard ratio for all-cause mortality was 1.25 for individuals with LDL-C concentrations of less than 70 mg/dL and 1.15 for LDL-C concentrations of more than 189 mg/dL.
The concentration of LDL-C associated with the lowest risk of all-cause mortality was 140 mg/dL in the overall population and in individuals not receiving lipid lowering treatment, compared with 89 mg/dL in individuals receiving lipid lowering treatment. Similar results were seen in men and women, across age groups, and for cancer and other mortality, but not for cardiovascular mortality.11
More evidence supports the link between LDL cholesterol levels and an increased risk of intracerebral hemorrhage (ICH). Results from a large, prospective longitudinal study show individuals with LDL below 70 mg/dL had a 65% increased likelihood of ICH over 9 years. Furthermore, the participants with LDL below 50 mg/dL had 169% greater risk compared with their counterparts who had levels in the 70 to 99 mg/dL range.[6]
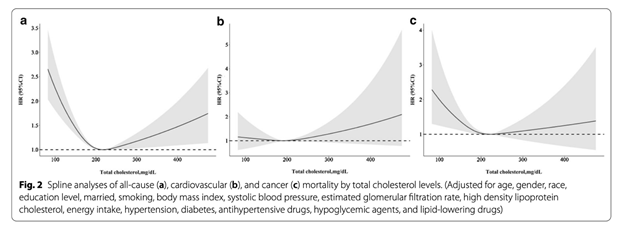
In a U.S. study, researchers evaluated the effect of total cholesterol levels on all-cause, cardiovascular disease (CVD), and cancer mortality.
All data analyzed were obtained from the National Health and Nutrition Examination Survey 1999-2014. The sample studied comprised 14,662 men and 16,025 women, categorized as 25,429 adults aged 18-65 and 5,258 adults over 65 years old. A total of 2,570 deaths were recorded. All-cause, cardiovascular, and cancer mortality showed U-curve associations after adjusting for confounding variables in the restricted cubic spline analysis.
Hazard ratios (HRs) of all-cause and cancer mortality were particularly negatively related to TC levels in the lower range < 200 mg/dL, especially in the range < 120 mg/dL. However, the HRs of cardiovascular disease mortality in the range < 120 mg/dL were the lowest. In the upper range, a TC range of ≥ 280 mg/dL was correlated with mortality as a result of CVD and cancer.
The lowest cumulative survival rate of all-cause mortality was recorded in the lowest TC-level group, while the lowest cumulative survival rate of CVD mortality was recorded in the highest TC-level group.
Normal to Slightly High Cholesterol is Associated with Longer Life
In contrast to the negative health effects of low cholesterol levels, population studies in Japan show that people of all ages with higher cholesterol live longer.[8]
Overall, an inverse trend is found in Japan between all-cause mortality and total LDL cholesterol levels: mortality is highest in the lowest cholesterol group without exception. If limited to elderly people, this trend is universal. Elderly people with the highest cholesterol levels have the highest survival rates irrespective of where they live in the world.
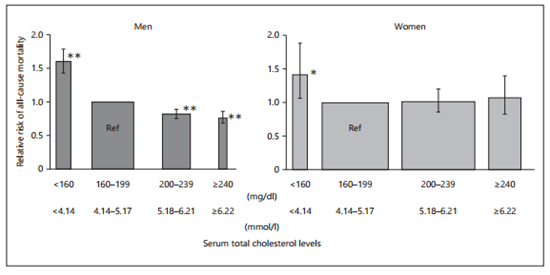
The chart above shows all-cause mortality by cholesterol levels, men on the left, women on the right.
Current guidelines call for keeping cholesterol at 200 mg/dl or lower, yet higher levels are associated with lower death rates.
What about outside Japan? The following chart shows cumulative all-cause mortality of people older than 85 in Leiden, The Netherlands, by cholesterol level.
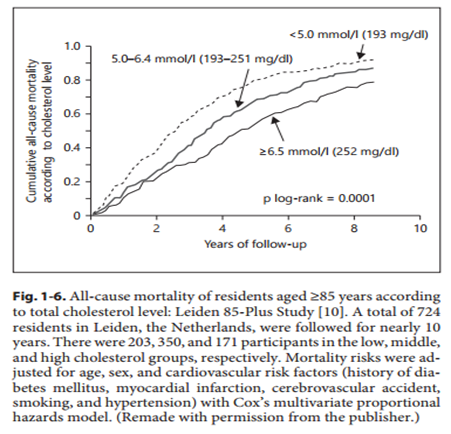
The cohort with an average cholesterol of 252 mg/dl, the highest, had the lowest death rates.
The following shows data from elderly people in Finland. Those with cholesterol greater than 232 mg/dl had the lowest death rates.
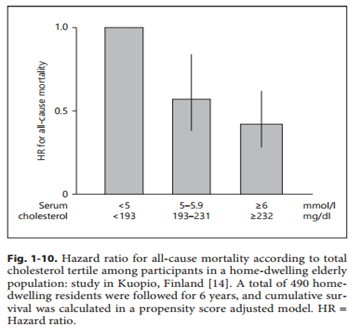
The data from Japan is for all ages; the data from outside Japan is for the elderly. What about the data for all ages, outside of Japan? The authors believe that the presence of people with familial hypercholesterolemia, which causes a very high cholesterol level and which raises the risk of death, in the highest cholesterol categories, accounts for higher death rates in those categories. They also argue that cholesterol levels in that disorder are not the cause of increased death rates.
A recent review in the prominent medical journal BMJ regarding LDL cholesterol (the risk marker considered most significant) found either no association or an inverse association between LDL and death rates.[9]
A 2017 study found a 30% lower rate of all-cause mortality in people over 60 with high cholesterol.[10] Compared to normal total cholesterol (<5.18 mmol/l), borderline-high (5.18–6.21 mmol/l) and high (≥6.22 mmol/l) total cholesterol were associated with a decreased risk of all-cause mortality.
The Honolulu Heart Program was one of the first studies to find this inverse relation between total cholesterol and death rates in elderly people aged 71 to 93. It found that compared to the lowest quartile (fourth) of cholesterol levels, increasing quartiles of cholesterol had 28%, 40%, and 35% decreased death rates, respectively.
Furthermore, the Honolulu study seems to provide evidence that actually raising cholesterol is protective, since only the group with low cholesterol concentration at both examinations had a significant association with mortality. These data cast doubt on the scientific justification for lowering cholesterol to very low concentrations (<180 mg/dl) in elderly people.”[11]
In a low 10-year risk cohort with long-term follow-up, LDL-C and non-HDL-C ≥160 mg/dL were independently associated with a 50% to 80% increased relative risk of CVD mortality.[12]
A 2019 study found that for most age groups total cholesterol levels had U-curve associations with mortality with lowest mortality being between 210-249 mg/dL.[13]
A very meaningful analysis compared total mortality rates to LDL cholesterol levels which found no statistically significant relationship.
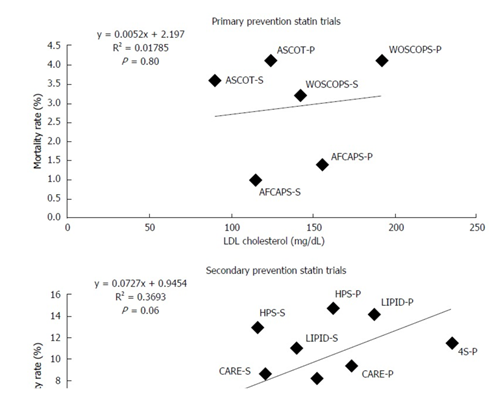
Comparison of mortality rates to low-density lipoprotein cholesterol levels using the randomized clinical trials.[14]
Mortality Benefits with Statins are Inconsistent
Although a number of statin trials have reported a mortality benefit, quite a few have not. A corollary to the cholesterol hypothesis posits that patients at highest risk should derive the greatest benefit from cholesterol lowering. However, statin trials in the elderly (PROSPER), in patients with heart failure (CORONA, GISSI-HF), and in patients with renal failure (4D, AURORA, SHARP) have all failed to demonstrate a mortality benefit.[15][16]
A Cochrane meta-analysis of 18 cholesterol-lowering trials (some with statins) in patients with peripheral arterial disease also failed to demonstrate a mortality benefit.[17]
Two different Cochrane studies on statins and mortality do not support statin as a preventive treatment to reduce all-cause mortality. One meta-analysis of 11 statin trials for high-risk primary prevention similarly failed to demonstrate a mortality benefit.[18]
Another Cochrane meta-analysis of statin usage after acute coronary syndromes concluded there was no mortality benefit.[19]
Some people do appear to benefit from statins. But consider this: The Cholesterol Treatment Trialists (CTT) performed a meta-analysis of 27 statin trials and concluded that statins were beneficial in reducing cardiovascular events.[20] However, when the same 27 trials were assessed for mortality outcomes, no benefit was seen.[21]
I believe that some high-risk people with extremely high cholesterol can benefit from a statin, but many do not. In particular, statins may impose more risk than benefit for the elderly. I also strongly believe that everything we do from a health perspective should be with the goal of helping people live better and live longer. This is the focus of Mederi-Care which is “Slow,” “Gentle,” “Unitive,” and “Nature-based.” Thus, our motto is, “Together we heal.”
The Role of Lipids in Chronic Diseases and Human Longevity
Digging deeper into the role of lipids and longevity, clinicians typically evaluate triglyceride and cholesterol levels to assess the risk of cardiovascular disease. Larger lipoprotein particle size and low triglyceride levels have been identified as markers of human longevity. Research shows that specific lipid molecular species, such as ether-linked phospholipids, may be selectively altered by aging.[22]
Low density lipoproteins are the main carriers of sphingomyelins and ceramides, while high density lipoproteins are mostly loaded with ether phosphocholines, partly explaining their opposing roles in atherogenesis. The identification of specific lipid species in aging diseases and longevity would help clarify how these lipids alter health and influence longevity. For instance, ether phosphocholines PC (O-34:1) and PC (O-34:3) have been positively associated with longevity and negatively with diabetes.[23]
Mitochondria and the endoplasmic reticulum accumulate high amounts of ether-phosphatidylcholine and ether-phosphatidylethanolamine. Mitochondria play an important role in ether lipid metabolism and intracellular ether lipid trafficking.[24]
Cholesteryl esters, the intracellular storage form and intravascular transport form of cholesterol, can exist in crystal, liquid crystal and liquid states.[25] Centenarians tend to have a unique difference in the alkyl and alkenyl cholesterol ethers.
- Centenarians have higher level of alkyl forms derived from phosphatidylcholine.
- Centenarians show decreased alkenyl forms from phosphatidylethanolamine.
- Ether lipids from centenarians are more resistant to lipid peroxidation.
- Ether lipid signature expresses an optimized trait associated with exceptional human longevity.[26],[27],[28]
- Research shows a nonlinear association of total cholesterol level with all-cause, cancer, and CVD mortality in the American population, suggesting that too low or too high serum total cholesterol levels might correlate with adverse outcomes.[29]
- Low and high levels of LDL-C are both associated with an increased risk of all-cause mortality. According to a recent study, the lowest risk of all-cause mortality was found at an LDL-C concentration of 140 mg/dL,[30] far above the standard-of-care guidelines.
Insulin Like Growth Factor-1 (IGF-1) as a New Biomarker of Longevity
Other biomarkers of longevity include growth hormone (GH) and the insulin-like growth factor-1 (IGF-1). These somatotropic hormones regulate cellular homeostasis and play significant roles in cell differentiation, function, and survival. In mammals, these hormones peak during puberty and decline gradually during adulthood and aging. GH and IGF-1 regulate mitochondrial mass and function and contribute to specific processes of cellular aging, including mitochondrial biogenesis, respiration and ATP production, oxidative stress, senescence, and apoptosis. The way these pathways intersect during aging is of particular interest to researchers.[31]
Of note is that lower levels of IGF-1 does not mean that IGF-1 is systemically lower. It may really reflect GH/IGF-1 hormone resistance, meaning the hormone isn’t getting into the cell because of some dysfunction involving the signaling, transportation, and/or receptor.
Laboratory studies on mice, flies, and worms show that when they have lower expression of a hormone similar to insulin called IGF-1 and closely related genes their lifespans are extended by as much as 50%.[32],[33],[34],[35],[36]
In one clinical study, a group of 184 people in their 90s were divided by IGF-1 levels into 2 groups: a low IGF-1 group and a high IGF-1 group. There were 93 people in the low IGF-1 group (mean 55 ng/mL) and 91 people in the high IGF-1 group (mean 121 ng/mL). Mean age was 96.8 years in the low group and 96.7 years in the high group.
In an analysis of overall mortality, very old women with IGF-1 levels below the median had significantly longer survival compared with females with levels above the median. This survival advantage was not observed in males. In both males and females with a history of cancer, lower IGF-1 levels predicted longer survival. This may be the first time that low IGF-1 levels have been shown to predict life expectancy in exceptionally long-lived individuals.
A separate study, published in the journal Aging Cell,evaluated the relationship between IGF-1 levels and longevity. The researchers tested 184 nonagenarians (individuals from 90 to 99 years old) and found that they have lower levels of IGF-1, leading the authors to conclude that “…low IGF-1 levels predict life expectancy in exceptionally long-lived individuals.”[37]
A reduction in IGF-1 receptor (IGFR) expression, which may mean, like insulin resistance, there is IGF-1 resistance with age is associated with decline in hippocampal-dependent learning and increased gliosis.[38]
Finally, Apo-E status appears to be a significant determinant of longevity that is imbedded in the genome at conception. The APOE gene comes in three different forms, and is involved in making a protein that helps carry cholesterol and other types of fat in the bloodstream. Depending on the form, it can convey protection or increased risk of cardiovascular disease and exerts continuing influence upon longevity across one’s entire lifespan—even beyond age 100.[39]
Optimize Evolutionary Adaptation and Strengthen Traits Associated with Longevity
Since the time of Darwin, evolutionary biologists have wondered why the lifespans of different species vary so significantly. A new model now suggests that the life expectancy of any given species is a function of evolutionary pressures — a conclusion that hints at the potential for powerful interventions in humans to extend lifespan and improve quality of life.
For example, one theory suggests that rather than trying to repair the processes of aging, we can try to trick the body into thinking it is younger. That way, the body will work to repair itself.[40]
It turns out one way to trick the body is to continue to be physically active. The less we do, the faster we age. Research shows that the cells of those who sit more than 10 hours per day are biologically eight years older than those who are less sedentary.[41]
Conventional medicine efforts to prevent cardiovascular disease have emphasized the benefits of lowering cholesterol as the single most important treatment. However, overlooked is the fact that numerous studies of cholesterol lowering have failed to demonstrate a mortality benefit, and the fact that the benefits of statins have been overstated.
Theories of atherosclerosis are multifactorial, including a more in-depth understanding of cholesterol (such as LDL particle number, LDL particle size and LDL Ox). However, most are independent of cholesterol metabolism, which is the true key to future preventive strategies.
Meanwhile, the Mediterranean diet has consistently lowered cardiovascular events and mortality in numerous studies—but does not typically lower cholesterol levels.
Understanding the biomarkers of the longest-lived individuals such as cholesterol, growth hormone, and IGF-1 can provide insight into longevity and perhaps offer ways to extend life span. At the same time, it’s clear that we should take simple lifestyle measures that are proven to improve health and optimize lifespan.
BUDDHA SAID:
Believe nothing just because a so-called wise person said it.
Believe nothing just because a belief is generally held.
Believe nothing just because it is said in ancient books.
Believe nothing just because it is said to be of divine origin.
Believe nothing just because someone else believes it.
Believe only what you yourself test and judge to be true.
“The Lord is tenderness and pity, slow to anger, full of faithful love. The Lord is generous to all, his tenderness embraces all his creatures.” (Psalm 145 vv8-9) I invite all of us to take a moment in these fear-filled times to discover a new way of living, offering compassion for all and for our Mother, the Earth.
References
[1] Arosio B, Ferri E, Casati M, Mari D, Vitale G, Cesari M. The frailty index in centenarians and their offspring. Aging Clin Exp Res. 2019;31(11):1685–8. https://doi.org/10.1007/s40520-019-01283-7.
[2] Kolovou G, Kolovou V, Vasiliadis I, Wierzbicki AS, Mikhailidis DP. Ideal lipid profile and genes for an extended life span. Curr Opin Cardiol. 2011 Jul;26(4):348-55. doi: 10.1097/HCO.0b013e32834659d4. PMID: 21478743.
[3] Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham study. Ann Intern Med 1979; 90: 85-91 [PMID: 217290]
[4] DuBroff R, de Lorgeril M. Cholesterol confusion and statin controversy. World J Cardiol. 2015 Jul 26;7(7):404-9. doi: 10.4330/wjc.v7.i7.404. PMID: 26225201; PMCID: PMC4513492.
[5] Sung KC, Huh JH, Ryu S, Lee JY, Scorletti E, Byrne CD, Kim JY, Hyun DS, Ko SB. Low Levels of Low-Density Lipoprotein Cholesterol and Mortality Outcomes in Non-Statin Users. J Clin Med. 2019 Oct 1;8(10):1571. doi: 10.3390/jcm8101571. PMID: 31581520; PMCID: PMC6832139.
[6] McNamara, Damian Medscape, Low LDL Means Higher Hemorrhagic Stroke Risk, July 08, 2019, https://www.medscape.com/viewarticle/915359#vp_2; Ma C, Gurol ME, Huang Z, Lichtenstein AH, Wang X, Wang Y, Neumann S, Wu S, Gao X. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: A prospective study. Neurology. 2019 Jul 30;93(5):e445-e457. doi: 10.1212/WNL.0000000000007853. Epub 2019 Jul 2. PMID: 31266905; PMCID: PMC6693427.
[7] He GD, Liu XC, Liu L, Yu YL, Chen CL, Huang JY, Lo K, Huang YQ, Feng YQ. A nonlinear association of total cholesterol with all-cause and cause-specific mortality. Nutr Metab (Lond). 2021 Mar 10;18(1):25. doi: 10.1186/s12986-021-00548-1. PMID: 33691735; PMCID: PMC7945313.
[8] Hamazaki T, Okuyama H, Ogushi Y, Hama R. Towards a Paradigm Shift in Cholesterol Treatment. A Re-examination of the Cholesterol Issue in Japan. Ann Nutr Metab. 2015;66 Suppl 4:1-116. doi: 10.1159/000381654. Epub 2015 Apr 29. PMID: 25925499.
[9] Ravnskov, Uffe, et al. “Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review.” BMJ open 6.6 (2016): e010401.
[10] Liang, Y., Vetrano, D.L. & Qiu, C. Serum total cholesterol and risk of cardiovascular and non-cardiovascular mortality in old age: a population-based study. BMC Geriatr 17, 294 (2017). https://doi.org/10.1186/s12877-017-0685-z
[11] Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet. 2001 Aug 4;358(9279):351-5. doi: 10.1016/S0140-6736(01)05553-2. PMID: 11502313.
[12] Abdullah SM, Defina LF, Leonard D, Barlow CE, Radford NB, Willis BL, Rohatgi A, McGuire DK, de Lemos JA, Grundy SM, Berry JD, Khera A. Long-Term Association of Low-Density Lipoprotein Cholesterol With Cardiovascular Mortality in Individuals at Low 10-Year Risk of Atherosclerotic Cardiovascular Disease. Circulation. 2018 Nov 20;138(21):2315-2325. doi: 10.1161/CIRCULATIONAHA.118.034273. PMID: 30571575.
[13] Yi SW, Yi JJ, Ohrr H. Total cholesterol and all-cause mortality by sex and age: a prospective cohort study among 12.8 million adults. Sci Rep. 2019;9(1):1596. Published 2019 Feb 7. doi:10.1038/s41598-018-38461-y
[14] O’Keefe JH, Cordain L, Harris WH, Moe RM, Vogel R. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol. 2004;43:2142–2146.
[15] de Lorgeril M. In: Souccar T, editor. Cholesterol and statins. Vergèze, France: Sham science and bad medicine; 2014.
[16] Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Eur Heart J. 2011;32:1769–1818.
[17] Aung PP, Maxwell HG, Jepson RG, Price JF, Leng GC. Lipid-lowering for peripheral arterial disease of the lower limb. Cochrane Database Syst Rev. 2007;(4):CD000123.
[18] Ray KK, Seshasai SR, Erqou S, Sever P, Jukema JW, Ford I, Sattar N. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170:1024–1031.
[19] Vale N, Nordmann AJ, Schwartz GG, de Lemos J, Colivicchi F, den Hartog F, Ostadal P, Macin SM, Liem AH, Mills EJ, et al. Statins for acute coronary syndrome. Cochrane Database Syst Rev. 2014;9:CD006870.
[20] Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590
[21] Abramson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ. 2013;347:f6123.
[22] Kawanishi, N., Kato, Y., Yokozeki, K. et al. Effects of aging on serum levels of lipid molecular species as determined by lipidomics analysis in Japanese men and women. Lipids Health Dis 17, 135 (2018). https://doi.org/10.1186/s12944-018-0785-6
[23] Gonzalez-Covarrubias V. Lipidomics in longevity and healthy aging. Biogerontology. 2013 Dec;14(6):663-72. doi: 10.1007/s10522-013-9450-7. Epub 2013 Aug 15. PMID: 23948799.
[24] Kuerschner L, Richter D, Hannibal-Bach HK, et al. Exogenous ether lipids predominantly target mitochondria. PLoS One. 2012;7(2):e31342. doi:10.1371/journal.pone.0031342
[25] Ginsburg GS, Atkinson D, Small DM. Physical properties of cholesteryl esters. Prog Lipid Res. 1984;23(3):135-67. doi: 10.1016/0163-7827(84)90002-x. PMID: 6399750.
[26] Pradas I, Jové M, Huynh K, Puig J, Ingles M, Borras C, Viña J, Meikle PJ, Pamplona R. Exceptional human longevity is associated with a specific plasma phenotype of ether lipids. Redox Biol. 2019 Feb;21:101127. doi: 10.1016/j.redox.2019.101127. Epub 2019 Jan 29. PMID: 30711699; PMCID: PMC6357979.
[27] Jové M, Naudí A, Gambini J, Borras C, Cabré R, Portero-Otín M, Viña J, Pamplona R. A Stress-Resistant Lipidomic Signature Confers Extreme Longevity to Humans. J Gerontol A Biol Sci Med Sci. 2017 Jan;72(1):30-37. doi: 10.1093/gerona/glw048. Epub 2016 Mar 24. PMID: 27013396.
[28] Jové M, Mota-Martorell N, Pradas I, Galo-Licona JD, Martín-Gari M, Obis È, Sol J, Pamplona R. The Lipidome Fingerprint of Longevity. Molecules. 2020 Sep 22;25(18):4343. doi: 10.3390/molecules25184343. PMID: 32971886; PMCID: PMC7570520.
[29] He GD, Liu XC, Liu L, Yu YL, Chen CL, Huang JY, Lo K, Huang YQ, Feng YQ. A nonlinear association of total cholesterol with all-cause and cause-specific mortality. Nutr Metab (Lond). 2021 Mar 10;18(1):25. doi: 10.1186/s12986-021-00548-1. PMID: 33691735; PMCID: PMC7945313.
[30] Johannesen CDL, Langsted A, Mortensen MB, Nordestgaard BG. Association between low density lipoprotein and all cause and cause specific mortality in Denmark: prospective cohort study. BMJ. 2020 Dec 8;371:m4266. doi: 10.1136/bmj.m4266. Erratum in: BMJ. 2021 Feb 12;372:n422. PMID: 33293274; PMCID: PMC7722479.
[31] Poudel SB, Dixit M, Neginskaya M, Nagaraj K, Pavlov E, Werner H, Yakar S. Effects of GH/IGF on the Aging Mitochondria. Cells. 2020 Jun 2;9(6):1384. doi: 10.3390/cells9061384. PMID: 32498386; PMCID: PMC7349719.
[32] Bartke A, Chandrashekar V, Bailey B, et al. Consequences of growth hormone (GH) overexpression and GH resistance. Neuropeptides. 2002;36(2-3):201-8.
[33] Broughton SJ, Piper MD, Ikeya T, et al. Longer lifespan, altered metabolism, and stress resistance in Drosophila from ablation of cells making insulin-like ligands. Proc Natl Acad Sci U S A. 2005;102(8):3105-10.
[34] Sonntag WE, Csiszar A, deCabo R, et al. Diverse roles of growth hormone and insulin-like growth factor-1 in mammalian aging: progress and controversies. J Gerontol A Biol Sci Med Sci. 2012;67(6):587-98.
[35] Halaschek-Wiener J, Khattra JS, McKay S, et al. Analysis of long-lived C. elegans daf-2 mutants using serial analysis of gene expression. Genome Res. 2005;15(5):603-15.
[36] Kenyon C, Chang J, Gensch E, et al. A C. elegans mutant that lives twice as long as wild type. Nature. 1993;366(6454):461-4.
[37] Milman S, Atzmon G, Huffman DM, et al. Low insulin-like growth factor-1 level predicts survival in humans with exceptional longevity. Aging Cell. 2014;13(4):769-71.
[38] Logan S, Pharaoh GA, Marlin MC, Masser DR, Matsuzaki S, Wronowski B, Yeganeh A, Parks EE, Premkumar P, Farley JA, Owen DB, Humphries KM, Kinter M, Freeman WM, Szweda LI, Van Remmen H, Sonntag WE. Insulin-like growth factor receptor signaling regulates working memory, mitochondrial metabolism, and amyloid-β uptake in astrocytes. Mol Metab. 2018 Mar;9:141-155. doi: 10.1016/j.molmet.2018.01.013. Epub 2018 Feb 2. PMID: 29398615; PMCID: PMC5870102.
[39] Hazzard WR. What heterogeneity among centenarians can teach us about genetics, aging, and longevity. J Am Geriatr Soc. 2001 Nov;49(11):1568-9. doi: 10.1046/j.1532-5415.2001.4911256.x. PMID: 11890602.
[40] Justin Werfel, Donald E. Ingber, and Yaneer Bar-Yam, Programed Death is Favored by Natural Selection in Spatial Systems, Phys. Rev. Lett. 114, 238103 – Published 12 June 2015
[41] Aladdin H. Shadyab et al. Associations of Accelerometer-Measured and Self-Reported Sedentary Time With Leukocyte Telomere Length in Older Women. American Journal of Epidemiology, January 2017 DOI: 10.1093/aje/kww196

Why this guy is the best healer. A terrific analysis.
Would add that hormones are made from cholesterol. Hormones are anabolic, lowering hormones is catabolic. Testosterone levels drop 20% in my male patients who come in on statins.
The brain is 53% cholesterol. So statins, which impair cognitive function (75% in one study), almost certainly shrinks the brain.
A 10 year VA study not only found an 87% increase in diabetes with statins but also a marked increase in… obesity!
In my diabetic patients, neuropathy is more commonly caused by statins than diabetes; the neuropathy improves with stopping statins. A 2003 study in Neurology showed a 16-fold increase in polyneuropathy; after two years, this was 26-fold.
What a marvelous comprehensive blog .