“When going thru hell, keep going.” Winston Churchill
Depression is one of the most common mental illnesses and can affect anyone at any age. Characterized by anhedonia (the inability to feel pleasure), despair, and pessimism, depression has high morbidity and recurrence.[1] Overall, more than 50% of the general population in middle- and high-income countries will suffer from at least one mental disorder at some point in their lives. This is obviously a major public health problem with significant consequences for society.[2] We need clear guidelines as to what does and doesn’t work for treating depression.

So, just how effective are antidepressant drugs? A 2016 analysis of multiple scientific studies sparked enormous scientific and public controversy by stating that the placebo effect is responsible for the apparent clinical effectiveness of antidepressants. How then do we explain the thousands of clinical trials providing compelling evidence for antidepressant effectiveness? If a meta-analysis compiles all the best published research, how could the analysis conclude that antidepressants don’t work much better than a sugar pill? (Hint: The key phrase here is “published research.”)
Published in the Lancet, the 2016 study denotes the “first comprehensive comparison of commonly prescribed antidepressant drugs so far.” In the study, medical researchers analyzed 34 pharmaceutical trials involving 5,260 participants ranging in age from 9 to 18 years.
Of 14 common antidepressants studied, only fluoxetine — best known under the brand name, Prozac — proved marginally more effective in treating major depression than a placebo. Alarmingly, venlafaxine, brand name Effexor, “was linked with an increased risk of engaging in suicidal thoughts or attempts” when compared to both placebo and five other medications.[3]
A recent 2021 study looked at 26 randomized trials of 6 to 18 year-olds of either sex and any ethnicity with clinically diagnosed major depressive disorder. Trials that compared the effectiveness of newer generation antidepressants with each other or with a placebo were included. Newer generation antidepressants included selective serotonin reuptake inhibitors; selective norepinephrine reuptake inhibitors; norepinephrine reuptake inhibitors; norepinephrine dopamine reuptake inhibitors; norepinephrine dopamine dis-inhibitors; and tetracyclic antidepressants.
Findings suggest that most newer antidepressants may reduce depression symptoms in a small and unimportant way compared with a placebo.[4]
What if Drug Companies are Manipulating the Results of Studies?
A recent article I read exposed some disturbing facts that need to be shared. It states that under the Freedom of Information Act, researchers applied to the FDA to obtain access to published and unpublished studies submitted by pharmaceutical companies to discover if the drug companies only published studies that showed a positive effect from antidepressants while concealing studies showing the drug didn’t work. What they found was shocking.[5]

According to an article from Scientific America, many antidepressant studies are found to be tainted by Pharma company influence. The latest study, published in the Journal of Clinical Epidemiology,[6] which evaluated 185 meta-analyses, found that one third of them were written by pharma industry employees. “We knew that the industry would fund studies to promote its products, but it’s very different to fund meta-analyses,” which “have traditionally been a bulwark of evidence-based medicine,” says John Ioannidis, an epidemiologist at Stanford University School of Medicine and co-author of the study. “It’s really amazing that there is such a massive influx of influence in this field. All of the major pharmaceutical companies were represented in the review, including GlaxoSmithKline; Eli Lilly and Co., maker of the popular antidepressant Prozac (fluoxetine); and Pfizer, which makes Zoloft (sertraline chloride).”[7]
“When published and unpublished data are combined, they fail to show a clinically significant advantage for antidepressant medication over a sugar pill. Not publishing negative results undermines evidence-based medicine and puts millions of patients at risk for using ineffective or unsafe drugs. This was the case for these antidepressant drugs.”[8]
In 2008, meta-analyses of antidepressant medications reported only modest benefits over placebo treatment, and when unpublished trial data was included, the benefit fell below accepted criteria for clinical significance.[9]
Antidepressants versus Placebos
Antidepressants are supposed to work by fixing a chemical imbalance, specifically, a lack of serotonin in the brain. Indeed, their supposed effectiveness is the primary evidence for the chemical imbalance theory. But analyses of the published data and the unpublished data that were hidden by drug companies reveals that most (if not all) of the benefits are due to the placebo effect.[10]
Even the small statistical difference between antidepressants and placebos may be an enhanced placebo effect, due to the fact that most patients and doctors in clinical trials successfully break blind. Instead of curing depression, popular antidepressants may induce a biological vulnerability making people more likely to become depressed in the future.[11]
A 2019 study that analyzed both the published and the unpublished clinical trial data are consistent in showing that most (if not all) of the benefits of antidepressants in the treatment of depression and anxiety are due to the placebo response, and the difference in improvement between drug and placebo is not clinically meaningful and may be due to breaking blind by both patients and clinicians.[12]
“Antidepressants offer substantial benefits to millions of people suffering from depression. If you are someone getting benefit from an antidepressant, by all means continue to take it. There is a strong therapeutic response to antidepressant medication, but it’s important to know that the response to placebo is almost as strong. To cast them as ineffective is inaccurate. Just because they may not work better than sugar pills doesn’t mean they don’t work.[13] The bottom line is that the overall effect of antidepressant medications is below recommended criteria for clinical significance. We also find that efficacy reaches clinical significance only in trials involving the most extremely depressed patients, but analyses of head-to-head comparisons suggest that they are not likely to be large enough to be of clinical importance.”[14]
The Downside of Antidepressant Drugs and Safer Alternatives
Among the side effects of antidepressants are sexual dysfunction in up to three-quarters of people, long-term weight gain, insomnia, nausea, and diarrhea.[15] Discontinuation of antidepressant treatment results in higher relapse rates among responders compared with treatment continuation.[16]
About one in five people experience withdrawal symptoms when they try to stop taking the medication. And perhaps more tragically, antidepressant drugs may increase the likelihood of future depressive episodes. Discontinuation symptoms can include a return and worsening of anxiety and depression.[17]

Antidepressant drugs have serious risks and should be considered only as a last resort in extreme cases after other safer alternatives have been exhausted. Health promoting alternatives need to be ample, robust, and consistent to successfully turn the tide and best efforts can be undermined when in the midst of an overwhelming depressive state. The upside of non-pharmaceutical interventions such as diet, exercise, time in nature, and herbal and nutritional medicine, is that not only are they free of the negative side effects associated with antidepressant drugs, but they actually result in enhanced libido and better sleep, decreased body fat, improved muscle tone, and a potentially longer and healthier life.
The Impact of the Pandemic on Mental Health in Adolescents
The COVID-19 era has seen a significant increase in depression, anxiety, agitation, restlessness, poor concentration, and insomnia.[19] School closures, social isolation and restriction of normal activities has taken a significant toll on children and can affect their development and wellbeing long after the crisis has passed.
A few weeks ago, Becker’s Hospital Review published a daily briefing titled, “Overrun with kids attempting suicide: Children’s Hospital Colorado (CHC) declares state of emergency.” The CEO and CMO of Children’s Hospital Colorado said pediatric emergency departments and inpatient units are being “overrun with kids attempting suicide and suffering from other forms of major mental health illness.”
In the last two years, CHC has seen a 90% increase in demand for behavioral health treatment. Isolation and stress amid the pandemic exacerbated low-level anxiety and depression among pediatric patients into suicide attempts, according to hospital officials. The number one most difficult requirement for hospitals in 2020, as written by the Joint Commission, was to reduce the risk for suicide.
Association of Screen Time and Depression in Adolescence
In a recent cohort study of 3826 adolescents, a within-person association, based on repeated measures, was found between social media and television use with symptoms of depression in adolescence. Use of social media and television in adolescents appear to enhance symptoms of depression and should therefore be taken into account when developing preventive methods.[20]
My Approach to Depression
Depression and anxiety are major public health problems and a primary contributing factor in chronic diseases including cancer, heart disease, obesity, and neurological diseases. Additionally, depression is associated with increased mortality, particularly in the elderly.
Most of the patients I see with chronic disease are also suffering from emotional stress, manifesting as depression, anxiety, grief, and insomnia. Depression and anxiety often occur together, and present with debilitating issues such as restlessness, fatigue, anger, concentration problems, tension, irritability, and sleep problems.
Too many doctors quickly diagnose depression without taking the time to listen to what the patient has to say, and they end up prescribing antidepressants without considering alternatives. We must involve ourselves with people in a more concerned and loving way, and that includes those of us in the healing profession.
I view depression and anxiety from a global perspective, using various diagnostic “lenses” to better understand all of the contributing factors, from the surrounding landscape to the internal landscape. In this way, I evaluate both the “host,” using energetic constitutional lens, the “microenvironment” using primary blood test testing, and the “external environment,” the space the person lives in and has been or is being affected by. I build supportive protocols tailored to the individual. This includes herbal formulas (including adaptogen and nervine-specific formulations), essential oils, nutrients, foods, and life-style changes that help create synergistic healing, with the goal of uplifting the life force, specifically the Vital Spirit.
“The power of God is hardwired and built-in at every point of nature. It can be found most directly in the hearts of humanity.” Orest Bedrig
Herbal Medicine Offers Support and Hope
Herbs have been used successfully for millennia to treat psychiatric disorders and generally have little to no harmful effects. Rather than producing a single action, as is the case with pharmaceutical drugs, herbal medicine strengthens and normalizes the endocrine, neurological and immunological systems through complex multi-tasking. Herbs affect multiple pathways and mediate cell behavior involved in all aspects of health, healing and longevity. In the modern world, it is ever important to expand our repertoire for alleviating depression and anxiety.
Many studies have reported that hypothalamus-pituitary-adrenal (HPA) axis hyperactivity is closely tied to depression, indicating the need for it to be considered in studies of depression etiology.[21] Clinical studies have found that the HPA axis of many patients with depression are hyperactive and return to a normal state following antidepressant treatment. Also, depression causes an increase in the adrenal index and volume of the pituitary and adrenal glands, with a decrease in the volume of the hippocampus.[22] Adaptogenic herbs specifically support the neuroendocrine system and help to normalize and strengthen the HPA axis, along with mitigating the effects stress may have on our organ systems.
There are many herbs I use to support mood and lift the spirit. Three of my favorites are hypericum, albizzia, and magnolia.
St. John’s wort (Hypericum perforatum)

Hypericum perforatum (St. John’s wort) has been used in traditional medicine for centuries for depressive disorders.[23] Called St. John’s wort because it blooms around the feast day of John the Baptist (June 24th), the plant grows prolifically along roadsides and in meadows. The bright yellow five-petaled flower resembles a halo; when pressed, the flowers release a crimson liquid that symbolized to early Christians the spilled blood of their beloved St. John.
Today, St. John’s wort extract is commonly used to treat mild to moderate depression. In energetic terms, it restores and uplifts the “Vital Spirit,” while clearing liver heat and toxins. I often refer to the herb as a neurological adaptogen stress-reliever and mood balancer.[24]
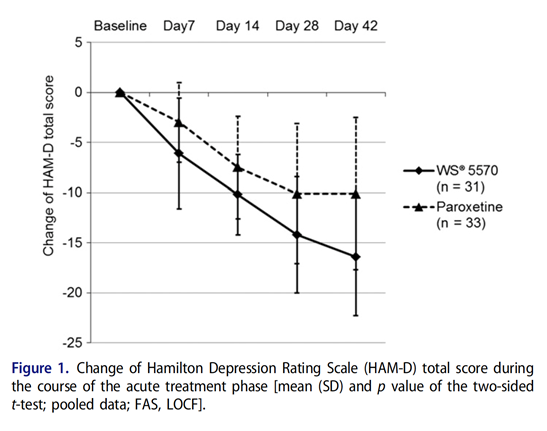
In research studies, hypericum perforatum extract (HPE) has been shown to be more effective than paroxetine (Paxil) in patients with a moderate major depressive episode.
A double blind, randomized trial compared the therapeutic efficacy of HPE with paroxetine in patients suffering from a major depressive episode with moderate symptom intensity. Depression was defined by a baseline Hamilton Depression Rating Scale (HAM-D) total score between 22 and 25. Patients received either 900 mg/d HPE or 20mg/d paroxetine for six weeks. Results showed that reductions in the HAM-D total score were significantly more pronounced in patients treated with HPE compared to paroxetine.
The researchers concluded that patients treated with HPE not only showed a reduction in depression severity score, but also yielded greater response and remission rates compared to patients treated with paroxetine.
Many more studies report similar findings. A review of 29 trials (5489 patients) showed that hypericum extract is more effective than placebo and is as effective as standard antidepressants in the treatment of major depression, with fewer adverse effects than standard antidepressant drugs.[26]
Albizzia (Albizzia julibrissin)
The flowers and bark of the mimosa tree (Albizzia julibrissin) are among the most valued of Chinese botanicals for relieving stress, insomnia and depression. In Traditional Chinese Medicine (TCM), albizzia is known as He huan hua, which in Mandarin means “consolidate happiness flower.” Albizzia is traditionally known as a Shen, or “spirit” tonic. According to TCM, albizzia enters the liver and heart channels where it regulates Qi, resolves depression, relieves stagnation, nourishes the heart and calms the mind.[27]
Albizzia bark extract (ABE) has been shown to enhance neurotransmitter secretion and regulation and has demonstrated anxiolytic-like effects.[28] In one animal study, ABE was shown to be an effective anxiolytic agent that acts via the serotonergic nervous system.[29] ABE orally administered at 200 mg/kg to mice showed an antidepressant-like effect.[30] Albizzia has also exhibited nootropic (brain enhancing) effects by improving object recognition.[31]
In one laboratory study, the effect of albizzia aqueous leaf extract (ALE) was assessed using elevated plus-maze and forced swimming tests in animal models of anxiety and depression. Researchers found the administration of ALE exhibited significant anxiolytic- and antidepressant-like effects and also antioxidant potential in the rat amygdala.[32]
Magnolia bark (Magnolia grandiflora/officinalis)
Magnolia bark (Hou Po) is prescribed in Ttraditional Chinese Medicine for a variety of

mental disorders, including depression. Used for thousands of years for treating Qi stagnation in the stomach and spleen networks, magnolia bark relieves dampness and has an aromatic, uplifting quality. It is especially useful in cases of digestive disturbance caused by emotional distress.
Two biphenols, honokiol and magnolol, are the primary active compounds in magnolia bark. Honokiol is a GABA modulator and a CB1 agonist (both GABA and CB1 regulate neurotransmitters in the brain) and has been extensively researched for its role in moderating mood disorders.
In a recent laboratory study, researchers reported that the oral administration of honokiol and magnolol has shown antidepressant-like effects in the “chronic unpredictable mild stress model.”[33] Use of the elevated plus maze experiment activity and traction tests in mice revealed that seven daily treatments with 0.2 mg kg and higher doses of honokiol exerted an anxiolytic effect without change in motor activity or muscle tone.[34]
In another study, researchers evaluated the possible neuroprotective effect of a standardized M. officinalis bark extract (MOE) enriched in honokiol, and its effect on animal mood behavioral tests and an in vitro model of excitotoxicity.
The researchers tested the effect of MOE in different behavioral tests evaluating anxiety and depression and observed a selective anxiolytic-like effect. MOE showed neuroprotective effects by normalizing brain-derived neurotrophic factor release. The researchers also confirmed the involvement of CB1 by the co-administration of the CB1 antagonist, AM251. The researchers concluded that MOE could be considered an effective and safe anxiolytic candidate with neuroprotective activity.[35]
In a study evaluating the effects of hononkiol on stress related depression, researchers injected laboratory rodents with corticosterone. Treatment with honokiol resulted in greater glucocorticoid receptor mRNA expression, greater glucocorticoid receptor-positive expression, and a greater ratio of glucocorticoid receptor to the mineralocorticoid receptor in the hippocampus. Moreover, honokiol treatment led to lower levels of interleukin-1β in serum and the positive expression of the interleukin-1β receptor in the hippocampus.
These results demonstrate that the antidepressant-like mechanism of honokiol, which has effects on inflammatory factors, may act through restoring the typical activity of the hypothalamus-pituitary-adrenal axis by regulating the glucocorticoid receptor-mediated negative feedback mechanism and the balance between glucocorticoid and mineralocorticoid receptors.[36]
Botanical Medicine Calms the Mind and Strengthens the Body
One of the great benefits of botanical medicine is that plants have pleiotropic effects—which means that they have multiple benefits. For example, when we’re treating anxiety and stress, we can at the same time be enhancing immunity, or bolstering cardiovascular health, or strengthening the body’s defenses against cancer.
Herbs are complex in that they bathe cells with hundreds of compounds, some of which may have very specific and direct ways in which they work, while others are non-specific and play a supportive role. Herbal nervines are unique in that they calm the sympathetic nervous system while enhancing the parasympathetic nervous system. Not only does this help us feel more relaxed, but it may also prevent illness and enable us to live a healthier and longer life.
My perspective is that healing is a mystical art form that engages the heart, working in harmony with the scientific aspect of medicine, which engages the mind. The heart cannot serve the mind, but the mind must serve the heart.
“If you give up your imagination,
if you give up your ability to create
for the wages of a good job,
then you might give up that which predicates us
as human beings,
the ability to create our own lives.”
–Godfrey Reggio
Instilling Hope
Using Karl Menninger’s and Paul Pruyser’s seminal writings, the view of hope can be based on an experience of benevolent connection.[37] Hope is always connected to spirituality and transfer beyond the physical plan. A connection has been highlighted in the literature that forms a relationship between spirituality and hope. Hope is generated through a dynamic and relational process of being hopeful together with others. Depression can

cause a dramatic situation of despair in which terrified and worried voices become the norm. Providing space and comfort and forming sacred meetings can replace these terrified voices with hopeful ones.[38] Hope, is intimately connected and founded in trust.[39]
Individual and Collective Spirituality
Individual and collective spirituality are encouraged, and spiritual development is unified and harmonized into the day-to-day life. We each inspire and energize behavior based on collective meaning and purpose rather than rewards and security, thus compelling each individual to transcend their self-interests for the sake of the mission and for the good of humanity.
“John Wesley’s Rule of Life”
Do all the good you can,
By all the means you can,
In all the ways you can,
In all the places you can,
At all the times you can,
To all the people you can,
As long as ever you can.
References
[1] LeMoult, J. and Gotlib, I. H. (2019) Depression: A cognitive perspective. Clinical Psychology Review 69, 51-66.
[2] Sebastian TrautmannJürgen RehmHans-Ulrich Wittchen The economic costs of mental disorders, BO Rep (2016)17:1245-1249https://doi.org/10.15252/embr.201642951
[3] Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, Coghill D, Zhang Y, Hazell P, Leucht S, Cuijpers P, Pu J, Cohen D, Ravindran AV, Liu Y, Michael KD, Yang L, Liu L, Xie P. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. 2016 Aug 27;388(10047):881-90. doi: 10.1016/S0140-6736(16)30385-3. Epub 2016 Jun 8. PMID: 27289172.
[4] Hetrick SE, McKenzie JE, Bailey AP, Sharma V, Moller CI, Badcock PB, Cox GR, Merry SN, Meader N. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. 2021 May 24;5(5):CD013674. doi: 10.1002/14651858.CD013674.pub2. PMID: 34029378; PMCID: PMC8143444.
[5] Smith, George, Lifestyle And Behaviour, Core Spirit member since Dec 24, 2020
https://corespirit.com/articles/exposed-antidepressants-are-no-more-effective-than-placebo, retrieved June 24, 2021
[6] Ebrahim S, Bance S, Athale A, Malachowski C, Ioannidis JP. Meta-analyses with industry involvement are massively published and report no caveats for antidepressants. J Clin Epidemiol. 2016 Feb;70:155-63. doi: 10.1016/j.jclinepi.2015.08.021. Epub 2015 Sep 21. PMID: 26399904.
[7] https://www.scientificamerican.com/article/many-antidepressant-studies-found-tainted-by-pharma-company-influence/ retrieved June 28, 2021
[8] Smith, George, Lifestyle And Behaviour, Core Spirit member since Dec 24, 2020
https://corespirit.com/articles/exposed-antidepressants-are-no-more-effective-than-placebo; retrieved June 24, 2021
[9] Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 2008 Feb;5(2):e45. doi: 10.1371/journal.pmed.0050045. PMID: 18303940; PMCID: PMC2253608.
[10] Kirsch I. Antidepressants and the Placebo Effect. Z Psychol. 2014;222(3):128-134. doi: 10.1027/2151-2604/a000176. PMID: 25279271; PMCID: PMC4172306.
[11] Kirsch I. The emperor’s new drugs: medication and placebo in the treatment of depression. Handb Exp Pharmacol. 2014;225:291-303. doi: 10.1007/978-3-662-44519-8_16. PMID: 25304538.
[12] Kirsch I. Placebo Effect in the Treatment of Depression and Anxiety. Front Psychiatry. 2019 Jun 13;10:407. doi: 10.3389/fpsyt.2019.00407. PMID: 31249537; PMCID: PMC6584108.
[13] Smith, George, Lifestyle And Behaviour, Core Spirit member since Dec 24, 2020
https://corespirit.com/articles/exposed-antidepressants-are-no-more-effective-than-placebo, retrieved June 24, 2021
[14] Hansen RA, Gartlehner G, Lohr KN, Gaynes BN, Carey TS (2005) Efficacy and safety of second-generation antidepressants in the treatment of major depressive disorder. Ann Intern Med 143: 415–426.
[15] https://www.healthline.com/health/antidepressant-side-effects retrieved June 30, 2021
[16] Batelaan N M, Bosman R C, Muntingh A, Scholten W D, Huijbregts K M, van Balkom A J L M et al. Risk of relapse after antidepressant discontinuation in anxiety disorders, obsessive-compulsive disorder, and post-traumatic stress disorder: systematic review and meta-analysis of relapse prevention trials BMJ 2017; 358 :j3927 doi:10.1136/bmj.j3927
[17] Going off antidepressants March 20, 2020, Harvard health Publishing, https://www.health.harvard.edu/diseases-and-conditions/going-off-antidepressants, retrieved June 30, 2021
[18] Smith, George, Lifestyle And Behaviour, Core Spirit member since Dec 24, 2020
https://corespirit.com/articles/exposed-antidepressants-are-no-more-effective-than-placebo; retrieved June 24, 2021
[19] Copelan, Russell MD June 2, 2021, Suicide Continues to Get Sad Before It Gets Sadder — Novel research and definitions are essential to reversing bleak trends, Suicide Continues to Get Sad Before It Gets Sadder | MedPage Today
[20] Elroy Boers, PhD; Mohammad H. Afzali, PhD; Nicola Newton, PhD; Patricia Conrod, PhD Association of Screen Time and Depression in Adolescence JAMA Pediatr. 2019;173(9):853-859. doi:10.1001/jamapediatrics.2019.1759, Published online July 15, 2019.
[21] Galts, C. P. C., Bettio, L. E. B., Jewett, D. C., Yang, C. C., Brocardo, P. S., Rodrigues, A. L. S., Thacker, J. S. and Gil-Mohapel, J. (2019) Depression neurodegenerative diseases: Common mechanisms and current treatment options. Neuroscience and Biobehavioral Reviews 102, 56-84.
[22] Gong, M., Han, B., Wang, S., Liang, S. and Zou, Z. (2016) Icariin reverses corticosterone-induced depression-like behavior, decrease in hippocampa derived neurotrophic factor (BDNF) and metabolic network disturbances revealed by NMR-based metabonomics in rats. Journal of Pharmaceutical a Biomedical Analysis 123, 63-73.
[23] Linde K, Mulrow CD, Berner M, Egger M. St John’s wort for depression. Cochrane Database Syst Rev. 2005 Apr 18;(2):CD000448.
[24] Naunyn Schmiedebergs, BMC Complementary and Alternative Medicine 2011, 11:7 http://www.biomedcentral.com/1472-6882/11/7, Arch Pharmacol. 2011 Apr;383(4):415-22. Epub 2011 Feb 19
[25] Erich Seifritz, Martin Hatzinger, Edith Holsboer-Trachsler, Efficacy of Hypericum extract WSVR 5570 compared with paroxetine in patients with a moderate major depressive episode – a subgroup analysis, INTERNATIONAL JOURNAL OF PSYCHIATRY IN CLINICAL PRACTICE, 2016 VOL. 20, NO. 3, 126–132 http://dx.doi.org/10.1080/13651501.2016.1179765
[26] Linde K, Berner MM, Kriston L. St John’s wort for major depression. Cochrane Database Syst Rev. 2008 Oct 8;2008(4):CD000448. doi: 10.1002/14651858.CD000448.pub3. PMID: 18843608; PMCID: PMC7032678.
[27] Bensky, D. and Gamble, X. Chinese Herbal Medicine Materia Medica, Eastland Press, Seattle, WA (1993)
[28] J.W. Jung, J.H. Cho, N.Y. Ahn, H.R. Oh, S.Y. Kim, C.G. Jang and J.H. Ryu. Effect of chronic Albizzia julibrissin treatment on 5-hydroxytryptamine1A receptors in rat brain. Pharmacol. Biochem. Behav. 81 (2005), pp. 205–210.
[29] W.K. Kim, J.W. Jung, N.Y. Ahn, H.R. Oh, B.K. Lee, J.K. Oh, J.H. Cheong, H.S. Chun and J.H. Ryu. Anxiolytic-like effects of extracts from Albizzia julibrissin bark in the elevated plusmaze in rats. Life Sci. 75 (2004), pp. 2787–2795.
[30] Kim JH, Kim SY, Lee SY, Jang CG. Antidepressant-like effects of Albizzia julibrissin in mice: involvement of the 5-HT1A receptor system. Pharmacol Biochem Behav. 2007 May; 87(1): 41-7. Epub 2007 Apr 6.
[31] Chintawar SD, Somani RS, Kasture VS, Kasture SB. Nootropic activity of Albizzia lebbeck in mice. J Ethnopharmacol 2002;81:299–305.
[32] Beppe GJ, Dongmo AB, Foyet HS, Dimo T, Mihasan M, Hritcu L. The aqueous extract of Albizia adianthifolia leaves attenuates 6-hydroxydopamine-induced anxiety, depression and oxidative stress in rat amygdala. BMC Complement Altern Med. 2015 Oct 19;15:374. doi: 10.1186/s12906-015-0912-0. PMID: 26481946; PMCID: PMC4615887.
[33] Qiang LQ, Wang CP, Wang FM, Pan Y, Yi LT, Zhang X, Kong LD. Combined administration of the mixture of honokiol and magnolol and ginger oil evokes antidepressant-like synergism in rats. Arch Pharm Res. 2009 Sep;32(9): 1281-92. Epub 2009 Sep 26.
[34] Kuribara H, Stavinoha WB, Maruyama Y. Honokiol, a putative anxiolytic agent extracted from magnolia bark, has no diazepam-like side-effects in mice. J Pharm Pharmacol. 1999 Jan;51(1): 97-103.
[35] Borgonetti V, Governa P, Manetti F, Miraldi E, Biagi M, Galeotti N. A honokiol-enriched Magnolia officinalis Rehder & E.H. Wilson. bark extract possesses anxiolytic-like activity with neuroprotective effect through the modulation of CB1 receptor. J Pharm Pharmacol. 2021 May 5:rgab067. doi: 10.1093/jpp/rgab067. Epub ahead of print. PMID: 33950239.
[36] Zhang B, Li Y, Liu M, Duan XH, Hu KL, Li LN, Yu X, Chang HS. Antidepressant-like mechanism of honokiol in a rodent model of corticosterone-induced depression. J Integr Neurosci. 2020 Sep 30;19(3):459-467. doi: 10.31083/j.jin.2020.03.172. PMID: 33070525.
[37] Allen JG. Hope in human attachment and spiritual connection. Bull Menninger Clin. 2013 Fall;77(4):302-31. doi: 10.1521/bumc.2013.77.4.302. PMID: 24354604.
[38] Espedal G. “Hope to See the Soul”: The Relationship Between Spirituality and Hope. J Relig Health. 2021 Mar 29. doi: 10.1007/s10943-021-01245-2. Epub ahead of print. PMID: 33779939.
[39] Allen JG. Preserving hope. Bull Menninger Clin. 2011 Spring;75(2):185-204. doi: 10.1521/bumc.2011.75.2.185. PMID: 21736417.

Thank you for your work, wisdom and words.
We are all here to help each other along, and your words speak my language, of our cooperation with each other and all of nature.
I believe this is a much healthier alternative. Although there are no serious side effects that come with the pharmaceutical drugs, I do want clarification on possible side effects of St. Johns Wort and Magnolia Bark.
I once took St. Johns Wort daily to reduce dental pain, and I became hypertensive. Though I know better alternatives now for inflammation, I still want to know about the side effects if taken daily.
Thank you.