The distribution of community outbreaks of the current global pandemic shows seasonal patterns associated with latitude, temperature, and humidity, which is similar to the behavior of seasonal viral respiratory tract infections.[1]

The seasonality of many viral infections is associated with a lack of sunlight, which results in low 25(OH)D concentrations and an uptick in diseases such as respiratory syncytial virus (RSV) infection.[2],[3],[4] While it’s obvious that winter in temperate climates interferes with sufficient exposure to ultra violet rays, the rainy season in tropical climates also results in low UVB exposure.
Several groups of researchers from different countries have found that the sickest patients often have the lowest levels of vitamin D, and that countries with higher death rates had larger numbers of people with vitamin D deficiency than countries with lower death rates.[5]
A recent study from Trinity College in Dublin, Ireland suggests that vitamin D deficiency is linked to higher mortality rates from COVID-19. Published in the Irish Medical Journal, the report analyzed vitamin D levels of older people in countries heavily affected by the coronavirus and found that places with high death rates from COVID-19, ironically including Italy and sunny Spain, had correspondingly high rates of vitamin D deficiency.[6]

Countries such as Norway and Finland—which have long, dark winters—have lower rates of vitamin D deficiency and lower mortality rates from COVID-19. To counteract the effects of insufficient sunshine, they eat a diet rich in vitamin D (cold water fish, whole milk dairy, and supplementary cod liver oil) and they commonly travel to southern Europe during the summer to sunbathe.
The “Spanish flu” of 1918–1919 claimed many lives. Researchers who looked back at the influenza pandemic found that patients with healthy vitamin D blood levels were less likely to die.[7] Vitamin D upregulates the production of human cathelicidin (LL-37), which has both antimicrobial and antiendotoxin activities. Vitamin D also reduces the production of proinflammatory cytokines, which could explain some of the benefit of vitamin D since H1N1 infection can give rise to a cytokine storm.11,12,13
Infection with SARS-CoV-2 results in a broad spectrum of disease, with more than 80% of patients having few or no symptoms. What is striking about COVID-19 is the enormous variation in the reported case fatality rate between countries and between regions in the same country. While these differences may in part be related to variations in case definitions, reporting and surveillance, they may also be attributed to underlying physiological reasons. It is likely that a number of factors, including age, co-morbidities, race, access to healthcare and genetic factors (and the complex interactions between these factors) along with vitamin D status determine the clinical course after exposure to SARS-CoV-2.
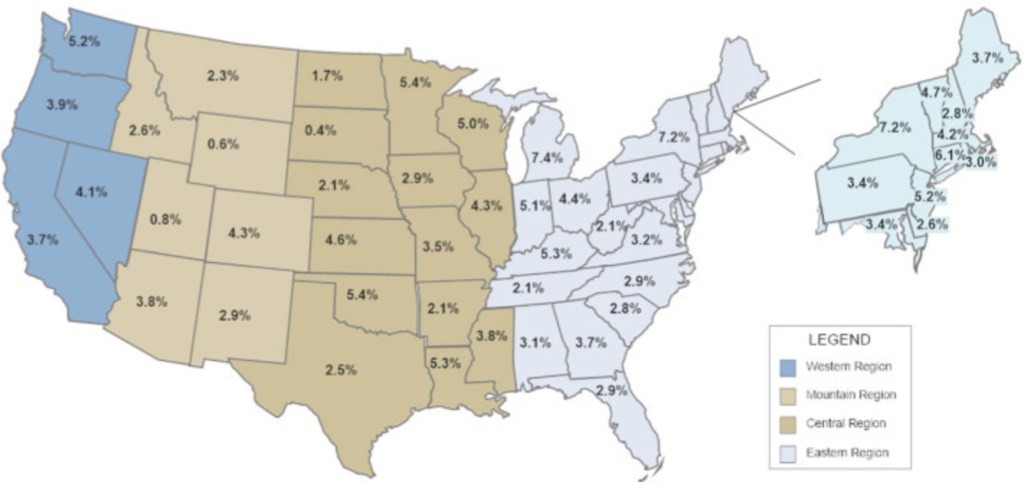
The reported case fatality rate (number of deaths/number of confirmed cases) for each of the 50 states in the USA as reported on 4/19/2020 by the Center for Systems Science and E.[8]
The Protective Effects of Vitamin D
Low levels of vitamin D can cause immune dysfunction, including lack of antibody production and increased risk of inflammation. With regard to respiratory function, low levels of vitamin D are associated with numerous pulmonary diseases, including acute lung injury and acute respiratory distress syndrome. Vitamin D and its receptors have been shown to protect epithelial barriers in various tissues, and offer protection against acute respiratory distress syndrome (ARDS) and fibrosis. [9] Vitamin D also appears to calm inflammation. In one study, providing vitamin D-deficient mice with vitamin D3 suppressed signs of lung inflammation.[10]
Vitamin D can lower the risk of infections by inducing cathelicidins and defensins that reduce viral replication rates and diminish concentrations of pro-inflammatory cytokines. These inflammatory compounds injure the lining of the lungs and increase the risk of pneumonia. Vitamin D enhances protection by increasing concentrations of anti-inflammatory cytokines.[11]
As an immune system modulator, vitamin D strongly influences immune function and is well known for its ability to enhance immune response when at optimal serum and tissue levels.
Modulating Cytokine Storms with Vitamin D
Respiratory failure from severe acute respiratory distress syndrome (SARDS) is the leading cause of mortality in COVID-19 patients.[12] Various studies show that vitamin D deficiency is widespread among the critically ill and suggest that vitamin D deficiency may contribute to the inflammatory basis of various illnesses. Even small amounts of vitamin D, about 500 IU, lowered inflammation by more than 25 percent in a small group of critically ill patients.[13] Another marker of inflammation (IL-6) was reduced even more.
This is important because studies show that detectable serum SARS-Cov-2 in COVID-19 patients was associated with elevated IL-6 concentration and poor prognosis. Elevated IL-6 may be part of a larger cytokine storm, and therefore could be a therapeutic target for critically ill patients with an excessive inflammatory response.[14]
There is a large, expanding body of research showing that vitamin D deficiency is linked to inflammatory processes and influences many diseases including heart disease, hypertension, obesity, osteoporosis, cancer, depression, chronic tension headaches, muscle weakness and type-2 adult onset diabetes.[15],[16]
In evaluating 25 randomized controlled trials with a total of 11,321 participants aged 0 to 95 years, vitamin D supplementation was shown to safely reduce the risk of acute respiratory tract infection among all participants. Patients who were vitamin D deficient and those not receiving bolus doses experienced the most benefit.[17]
While effective treatments for acute respiratory distress syndrome (ARDS) are lacking, mechanical lung ventilation can sustain adequate gas exchange in critically ill patients with respiratory failure due to ARDS. However, as a result of the phenomenon of ventilator-induced lung injury (VILI), there is an increasing need to seek beneficial therapies for ARDS.
- Recent studies have suggested the renin-angiotensin system (RAS), which consists of the ACE/Ang-II/AT1R axis and ACE2/Ang-(1-7)/MasR axis, plays a dual role in the pathogenesis of ARDS and VILI.
- ACE/Ang-II/AT1R axis has a deleterious action, whereas ACE2/Ang-(1-7)/MasR axis, as well as AT2R, in VILI and ARDS, plays a beneficial role.
- Targeting RAS components could improve outcomes in ARDS.[18]
Chronic vitamin D deficiency may induce renin-angiotensin system (RAS) activation lung fibrosis through activation of the RAS. Therefore, increasing evidence indicates that 25(OH)D may also be a negative endocrine regulator of the RAS, and may exert protective effects on inflammation-induced lung injury.[19]
In patients with chronic lung disease, vitamin D deficiency is common. An observational study notes a significant association between vitamin D deficiency and decreased pulmonary function tests in a large ambulatory population.[20] Conversely, people with higher levels of vitamin D (measured by circulating 25-hydroxyvitamin D) in the blood have improved cardiorespiratory fitness.[21]
Overall, vitamin D deficiency is commonly seen in intensive care patients and is related with poor clinical status at ICU admission.[22] The deficiency of 25-hydroxyvitamin D at the time of critical care initiation is a significant predictor of all-cause patient mortality in a critically ill patient population.
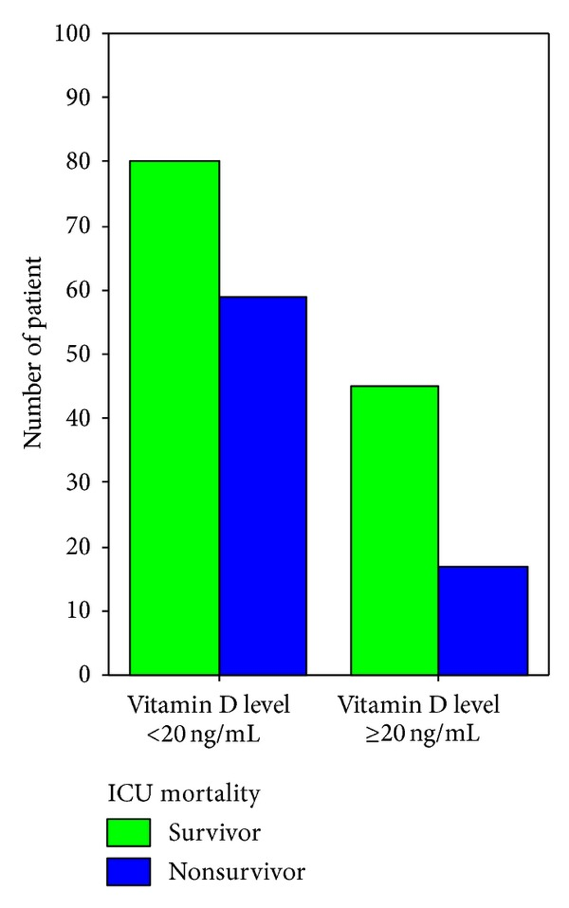
ICU mortality rate in vitamin D insufficient and sufficient patients (P = 0.027)[23]
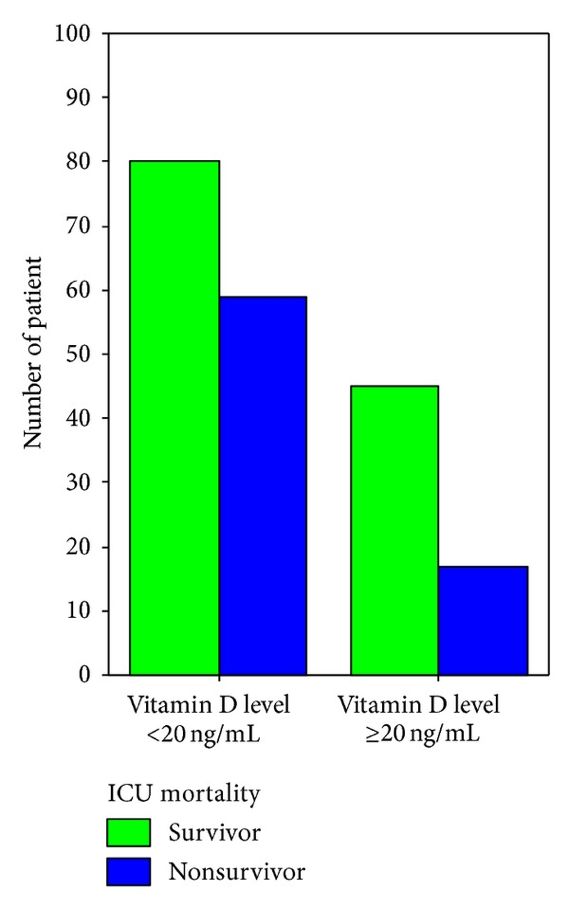
Applying invasive mechanical ventilation (MV) on admission in vitamin D insufficient and sufficient patients (P = 0.012).[24]
Vitamin D Lowers the Risk of Flu in Non-Vaccinated People
In a study of non-vaccinated people, vitamin D sufficiency was associated with a significantly lower risk of influenza. In this nested case-control study among Japanese workers, circulating 25-hydroxyvitamin D concentrations at baseline were not appreciably associated with influenza risk. Among participants who did not receive vaccination, however, researchers found a significantly decreased risk of influenza in the highest category of 25-hydroxyvitamin D concentration.[25]
Low Levels of Vitamin D Common in the Elderly
Research shows the prevalence of hypovitaminosis D in normal elderly persons ranges from 68.4% to 94%.[26]
Geriatric syndrome and physical performance impairment are commonly considered as multidimensional clinical conditions in older persons.29 This is characterized by the decline of functional, cognitive status and capacities of an elderly person suffering from exogenous and endogenous stressors. Low levels of vitamin D (25-OH) correlate with increased risk for depression, immune dysfunction, poor cognition, osteoporosis, cancer incidence and progression, and reduced quality-of-life.[27],[28]
Frailty is a multidimensional syndrome that leads to an increase of age-related disorders of several physiological systems along with a decline in cognitive abilities. Again, low levels of vitamin D (25-OH) are associated with increased risk for Frailty Syndrome.[29],[30]
The Relationship of Vitamin D Levels and Mortality
In a study of elderly (age >70 yr) female patients recruited from 95 nursing homes in Austria, researchers found that the majority are vitamin D deficient during winter and that there was an inverse association of 25(OH)D and mortality.[31]
Evidence from a meta-analysis of observational studies indicates inverse associations of circulating 25-(OH) D with risks of death due to cardiovascular disease, cancer, and other causes. Supplementation with vitamin D3 has been found to significantly reduce overall mortality among older adults.[32]
All-cause mortality is independently and inversely associated with serum 25(OH)D levels at levels less than 50 nmol/liter.[33]
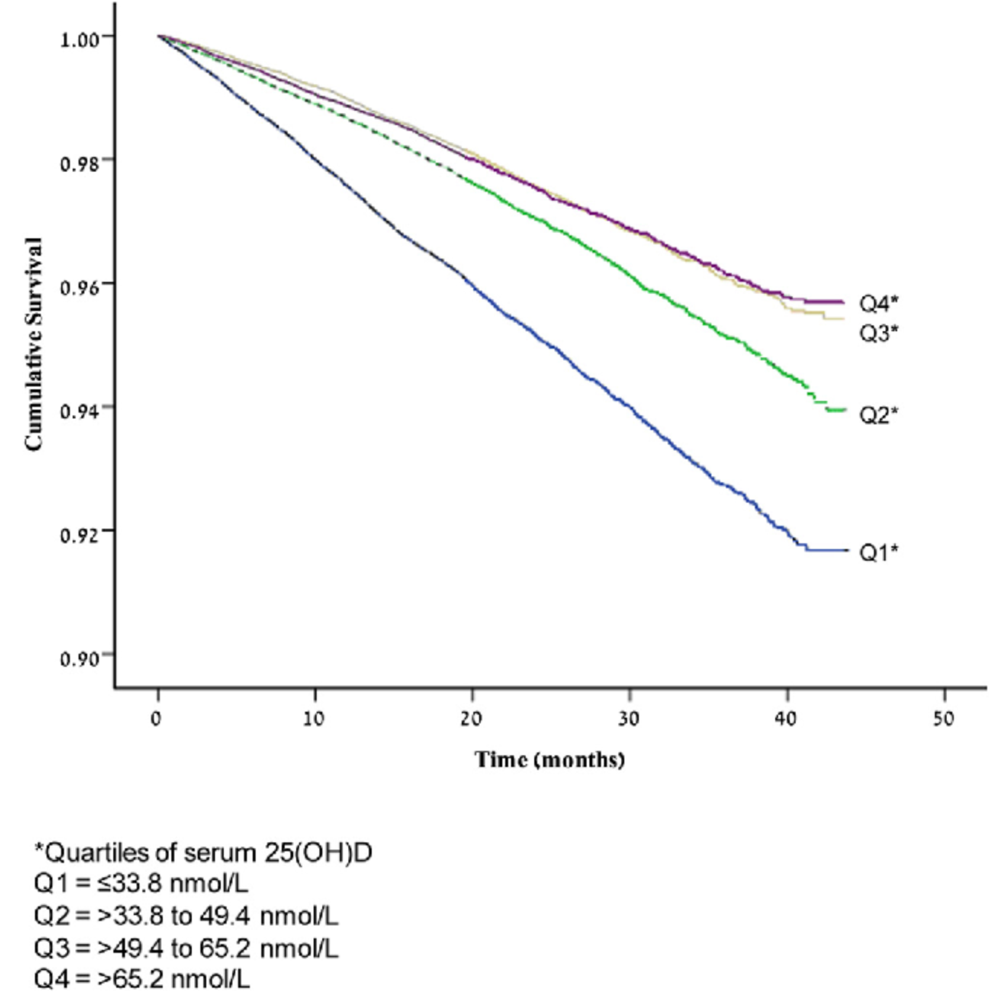
According to a study from Israel involving 182,152 participants over a 28.5-month period, low levels of vitamin D correlate with all-cause mortality.[34]
Appropriate levels of serum vitamin D are strongly correlated with cardiovascular health. In a study evaluating the connection between serum 25(OH)D levels, hypertension, and cardiovascular disease, researchers compared data from the 2001-2004 National Health and Nutrition Examination Survey with mortality data obtained through 2006. Concentrations of 25(OH)D as a continuous variable were inversely associated with the risk of mortality from all causes, including CVD mortality among adults with hypertension in the US.[35]
Another study involving 4,114 patients also demonstrated increased all-cause and CVD mortality in patients with 25(OH)D concentrations <20 ng/mL. Moreover, analysis suggested increased all-cause mortality at concentrations >40 ng/mL.[36] Other research indicates that 25-hydroxyvitamin D deficiency is associated with increased mortality in patients with chronic heart failure due to left ventricular systolic dysfunction.[37]
Low 25(OH)D and high PTH concentrations were associated with increased mortality in black and white community-dwelling older adults. Because 25(OH)D concentrations tend to be even lower in blacks, the potential impact of remediating low 25(OH)D concentrations is greater in blacks than whites.[38]
What is an Optimal Range for Vitamin D?
The US Institute of Medicine (IOM) recommendations for vitamin D based on a review of the evidence, concluded that:
- serum 25(OH)D <30 ng/mL is deficient
- serum 25(OH)D of 30–40 ng/mL may be ‘inadequate’
- serum 25(OH)D >40 ng/mL is ‘sufficient’ for almost the whole population (97.5%)[39]
• The goal should be to raise 25(OH)D concentrations above 40 ng/mL (100 nmol/L).
The Synergistic Benefits of Vitamin D & Vitamin K
I believe supplementing with vitamin D is essential for optimal health, but it should always be combined with vitamin K and a wholefood carotenoid complex, such as red palm oil. This trio has synergistic pleiotropic beneficial influences, especially in relation to immune response, cell-cycle functions, cardiovascular, and skeletal health.
The benefits of vitamin K have recently been widely shown to extend beyond blood homeostasis. A deficiency is implicated in chronic low-grade inflammatory diseases such as cardiovascular disease, osteoarthritis, dementia, cognitive impairment, mobility disability, and frailty.[40] A higher intake of vitamin K is associated with decreased serum levels of the inflammatory marker CRP (C-reactive protein).[41],[42],[43]
There are two main forms of vitamin K—K1, and K2. The main dietary source of vitamin K is K1 (phylloquinone). It plays a role in photosynthesis and is abundant in green leafy vegetables and algae. Vitamin K2 (menaquinone) occurs in foods in smaller amounts and mostly in butter, eggs, liver, cheese, and in fermented products. Fermented soybeans in the form of natto are especially rich in K2. In addition, a small amount of K2 is produced from beneficial bacteria in the large intestine.[44]

Observation shows that vitamin K status is reduced in patients with COVID-19 and is related to a poor prognosis. In addition, low vitamin K status seems to be associated with accelerated elastin degradation. Researchers suggest that an intervention trial is needed to assess whether vitamin K administration improves the outcome in patients with COVID-19.[45]
Of note is that although vitamin K is essential for proper blood clotting, no increase in hypercoagulation has been observed in individuals consuming doses above the recommended daily allowance of 75 micrograms vitamin K.[46]
Supplementing with Vitamin D
- It’s best to supplement with a food grown form that also includes a small amount of vitamin K (either K-1 or K-2, or both), and vitamin A.
- Simply taking extra vitamin D is not the correct approach. Instead, the appropriate amount must be provided to maintain serum levels in a healthy range 25 OH (>45 <80).
- Always check both forms of vitamin D; that means 25-OH and 1,25 dihydroxyvitamin (di OH). While 1,25 vitamin D is the most potent vitamin D metabolite, 25-OH vitamin D levels more accurately reflect vitamin D status because parathyroid hormone and other hormones do not influence it. If you only check 25-OH after supplementing with vitamin D, and the levels don’t increase, proceed by checking the 1,25 di OH level and the parathyroid hormone level. If these are either high normal, or elevated out-of-range, then you need to seek a professional skilled at normalizing vitamin D levels.
With all this said, I hope
and pray that somehow the pandemic will ultimately be a positive transformation
for us as individuals and for our healthcare system. Transformation is often
very unsettling, but we must demand that we move past this place of unhealthy
“normalcy” to a new place of renewed health and wellbeing. Stay informed and be
kind to one another, because together, we heal.
[1] Kara M, Ekiz T, Ricci V, Kara Ö, Chang KV, Özçakar L. ‘Scientific Strabismus’ or Two Related Pandemics: COVID-19 & Vitamin D Deficiency [published online ahead of print, 2020 May 12]. Br J Nutr. 2020;1‐20. doi:10.1017/S0007114520001749
[2] Nam, H.H.; Ison, M.G. Respiratory syncytial virus infection in adults. BMJ 2019, 366, l5021.
[3] Nassar, M.S.; Bakhrebah, M.A.; Meo, S.A.; Alsuabeyl, M.S.; Zaher,W.A. Global seasonal occurrence of middle east respiratory syndrome coronavirus (MERS-CoV) infection. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3913–3918.
[4] Paynter, S.; Ware, R.S.; Sly, P.D.; Weinstein, P.; Williams, G. Respiratory syncytial virus seasonality in tropical Australia. Aust. N. Z. J. Public Health 2015, 39, 8–10.
[5] Dohney, K., More Vitamin D, Lower Risk of Severe COVID-19?, WebMD, 5/19/2010, https://www.webmd.com/lung/news/20200518/more-vitamin-d-lower-risk-of-severe-covid-19?ecd=wnl_spr_051920&ctr=wnl-spr-051920_nsl-LeadModule_titl…retrieved 5/19/2020
[6] McCartney DM, Byrne DG. Optimisation of Vitamin D Status for Enhanced Immuno-protection Against Covid-19. Ir Med J. 2020;113(4):58. Published 2020 Apr 3. https://eurekalert.org/pub_releases/2020-05/tcd-vdd051220.php, Vitamin D determines severity in COVID-19 so government advice needs to change, NEWS RELEASE 12-MAY-2020
[7] Grant WB, Giovannucci, E, Dermato-Endocrinology: “The possible roles of solar ultraviolet-B radiation and vitamin D in reducing case-fatality rates from the 1918-1919 influenza pandemic in the United States.”
11 Paynter, S.; Ware, R.S.; Sly, P.D.; Weinstein, P.; Williams, G. Respiratory syncytial virus seasonality in tropical Australia. Aust. N. Z. J. Public Health 2015, 39, 8–10.
[8] Marik PE, Kory P, Varon J. Does vitamin D status impact mortality from SARS-CoV-2 infection? [published online ahead of print, 2020 Apr 29]. Med Drug Discov. 2020;100041. doi:10.1016/j.medidd.2020.100041
[9] Shi YY, Liu TJ, Fu JH, et al. Vitamin D/VDR signaling attenuates lipopolysaccharide‑induced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier. Mol Med Rep. 2016;13(2):1186‐1194. doi:10.3892/mmr.2015.4685
[10] Gorman S, Buckley AG, Ling KM, et al. Vitamin D supplementation of initially vitamin D-deficient mice diminishes lung inflammation with limited effects on pulmonary epithelial integrity. Physiol Rep. 2017;5(15):e13371. doi:10.14814/phy2.13371
[11] Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12(4):E988. Published 2020 Apr 2. doi:10.3390/nu12040988
[12] Ruan Q, Yang K, Wang W, Jiang L, Song J; Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020; (published online March 3.)
[13] Van den Berghe G, Van Roosbroeck D, Vanhove P, Wouters PJ, De Pourcq L, Bouillon R. Bone turnover in prolonged critical illness: effect of vitamin D. J Clin Endocrinol Metab. 2003;88(10):4623‐4632. doi:10.1210/jc.2003-030358
[14] Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality [published online ahead of print, 2020 Mar 29]. Int J Antimicrob Agents. 2020;105954. doi:10.1016/j.ijantimicag.2020.105954
[15] Lappe JM, Travers-Gustafson D, et al. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007. 85:1586 –1591.
[16] Prakash, S, Shah ND, et al. Chronic Tension-type Headache with Vitamin D Deficiency: Casual or Causal Association? Medscape article.
[17] Martineau, Adrian R et al. “Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data.” BMJ (Clinical research ed.) vol. 356 i6583. 15 Feb. 2017, doi:10.1136/bmj.i6583.
[18] Wang D, Chai XQ, Magnussen CG, et al. Renin-angiotensin-system, a potential pharmacological candidate, in acute respiratory distress syndrome during mechanical ventilation. Pulm Pharmacol Ther. 2019;58:101833. doi:10.1016/j.pupt.2019.101833
[19] Xu J, Yang J, Chen J, Luo Q, Zhang Q, Zhang H. Vitamin D alleviates lipopolysaccharide‑induced acute lung injury via regulation of the renin‑angiotensin system. Mol Med Rep. 2017;16(5):7432‐7438. doi:10.3892/mmr.2017.7546
[20] Gilbert CR, Arum SM, Smith CM. Vitamin D deficiency and chronic lung disease. Can Respir J. 2009;16(3):75‐80. doi:10.1155/2009/829130
[21] Amr Marawan, Nargiza Kurbanova, Rehan Qayyum. Association between serum vitamin D levels and car‐ diorespiratory fitness in the adult population of the USA. European Journal of Preventive Cardiology, 2018; 204748731880727 DOI: 10.1177/2047487318807279.
[22] Atalan HK, Güçyetmez B. Serum Vitamin D Level at ICU Admission and Mortality. Turk J Anaesthesiol Reanim. 2017;45(4):193‐196. doi:10.5152/TJAR.2017.60234
[23] Braun AB, Gibbons FK, Litonjua AA, Giovannucci E, Christopher KB. Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality. Crit Care Med. 2012;40(1):63‐72. doi:10.1097/CCM.0b013e31822d74f3
[24] Zhao G, Ford ES, Li C, Croft JB, Serum 25-hydroxyvitamin D levels and all-cause and cardiovascular disease mortality among US adults with hypertension: the NHANES linked mortality study. J Hypertens. 2012 Feb;30(2):284-9
[25] Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12(4):E988. Published 2020 Apr 2. doi:10.3390/nu12040988
[26] G.M. Kiebzak, N.L. Moore, S. Margolis, B. Hollis, C.G. KevorkianVitamin D status of patients admitted to a hospital rehabilitation unit. Relationship to function and progress, Am J Phys Med Rehabil, 86 (6) (2007), pp. 435-445
[27] L. Perna, U. Mons, M. Kliegel, H. BrennerSerum 25-hydroxyvitamin D and cognitive decline: a longitudinal study among nondemented older adults, Dement Geriatr Cognit Disord, 38 (2014), pp. 254-263
[28] H.A. Bischoff-Ferrari, E. Giovannucci, W.C. Willett, T. Dietrich, B. Dawson-Hughes, Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes Am J Clin Nutr, 84 (1) (2006), pp. 18-28
[29] Hammami S, Zarrouk A, Piron C, Almas I, Sakly N, Latteur V. Prevalence and factors associated with frailty in hospitalized older patients. BMC Geriatr. 2020;20(1):144. Published 2020 Apr 19. doi:10.1186/s12877-020-01545-4
[30] Wong YY, McCaul KA, Yeap BB, Hankey GJ, Flicker L. Low vitamin D status is an independent predictor of increased frailty and all-cause mortality in older men: the health in men study. J Clin Endocrinol Metab. 2013;98:3821–3828. doi: 10.1210/jc.2013-1702.
[31] Chowdhury R1, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, Khan H, Baena CP, Prabhakaran D, Hoshen MB, Feldman BS, Pan A, Johnson L, Crowe F, Hu FB, Franco OH. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies, BMJ. 2014 Apr 1;348:g1903. doi: 10.1136/bmj.g1903
[32] Cubbon RM, Lowry JE, Drozd M, Hall M, Gierula J, Paton MF, Byrom R, Kearney LC, Barth JH, Kearney MT, Witte KK. Vitamin D deficiency is an independent predictor of mortality in patients with chronic heart failure. Eur J Nutr. 2018 Aug 18. doi: 10.1007/s00394-018-1806-y.
[33] Braun AB, Gibbons FK, Litonjua AA, Giovannucci E, Christopher KB. Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality. Crit Care Med. 2012;40(1):63‐72. doi:10.1097/CCM.0b013e31822d74f3
[34] Saliba W, Barnett O, Rennert HS, Rennert G. The Risk of All-Cause Mortality Is Inversely Related to Serum 25(OH)D Levels. J Clin Endocrinol Metab. 2012 May 30.
[35] Zhao G, Ford ES, Li C, Croft JB, Serum 25-hydroxyvitamin D levels and all-cause and cardiovascular disease mortality among US adults with hypertension: the NHANES linked mortality study. J Hypertens. 2012 Feb;30(2):284-9
[36] Pilz S, Dobnig H, Tomaschitz A, Kienreich K, Meinitzer A, Friedl C, Wagner D, Piswanger-Sölkner C, März W, Fahrleitner-Pammer A. MODERN RESEARCH Low 25-hydroxyvitamin D is associated with increased mortality in female nursing home residents, J Clin Endocrinol Metab. 2012 Apr;97(4):E653-7.
[37] Eirik Degerud, Ottar Nygård, Stefan de Vogel, Rune Hoff, Gard Frodahl Tveitevåg Svingen, Eva Ringdal Pedersen, Dennis Winston Trygve Nilsen, Jan Erik Nordrehaug, Øivind Midttun, Per Magne Ueland, Jutta Dierkes, Plasma 25-Hydroxyvitamin D and Mortality in Patients With Suspected Stable Angina Pectoris, The Journal of Clinical Endocrinology & Metabolism, Volume 103, Issue 3, March 2018, Pages 1161–1170, https://doi.org/10.1210/jc.2017-02328
[38] Kritchevsky SB, Tooze JA, Neiberg RH, et al. 25-Hydroxyvitamin D, parathyroid hormone, and mortality in black and white older adults: the health ABC study. J Clin Endocrinol Metab. 2012;97(11):4156‐4165. doi:10.1210/jc.2012-1551
[39] Spiro A, Buttriss JL. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39(4):322‐350. doi:10.1111/nbu.12108
[40] Simes DC, Viegas CSB, Araújo N, Marreiros C. Vitamin K as a Diet Supplement with Impact in Human Health: Current Evidence in Age-Related Diseases. Nutrients. 2020;12(1):138. Published 2020 Jan 3. doi:10.3390/nu12010138
[41] Kidd PM. Vitamins D and K as pleiotropic nutrients: clinical importance to the skeletal and cardiovascular systems and preliminary evidence for synergy. Alt Med Rev. 2010 Sep. 15(3):199-222.
[42] Palmer CR, Blekkenhorst LC, Lewis JR, et al. Quantifying dietary vitamin K and its link to cardiovascular health: a narrative review. Food Funct. 2020;11(4):2826‐2837. doi:10.1039/c9fo02321f
[43] Monograph: Vitamin K2. Alt Med Rev. 2009. 14(3):284-293.
[44] Tamori A, Habu D, et al. Potential role of vitamin K(2) as a chemopreventive agent against hepatocellular carcinoma. Hepatol Res. 2007 Sep. 37 Supp (2):S303-307.
[45] Dofferhoff, A.S.; Piscaer, I.; Schurgers, L.J.; Walk, J.; van den Ouweland, J.M.; Hackeng, T.M.; Lux, P.; Maassen, C.; Karssemeijer, E.G.; Wouters, E.F.; Janssen, R. Reduced Vitamin K Status as A Potentially Modifiable Prognostic Risk Factor in COVID-19. Preprints 2020, 2020040457 (doi: 10.20944/preprints202004.0457.v1).
[46] Theuwissen, E.; Cranenburg, E.C.; Knapen, M.H.; Magdeleyns, E.J.; Teunissen, K.J.; Schurgers, L.J.; Smit, E.; Vermeer, C. Low-dose menaquinone-7 supplementation improved extra-hepatic vitamin K status, but had no effect on thrombin generation in healthy subjects. Br. J. Nutr. 2012, 108, 1652–1657

One Reply to “There’s No Substitute for Sunlight: The Essential Influence of Nature’s Sunshine Vitamin on Health”