Although Omicron is now 73% of all new cases in the US[1], I don’t feel we need to press the panic button. I have some hypotheses on the emergence of the Omicron variant that could put the brakes on the doom and gloom scenario we are all being fed.
According to a study published on December 16th, authored by more than 20 scientists at Columbia and the University of Hong Kong, a striking feature of the Omicron variant is the large number of spike mutations that pose a threat to the efficacy of current COVID-19 vaccines, vaccine boosters and antibody therapies.[2] The scientists express concern that the variant’s “extensive” mutations can “greatly compromise” the vaccine, even neutralizing it. The report said the booster shots prevent some of the neutralization, but the variant “may still pose a risk” for those with their third shot. “Even a third booster shot may not adequately protect against Omicron infection,” the study said.
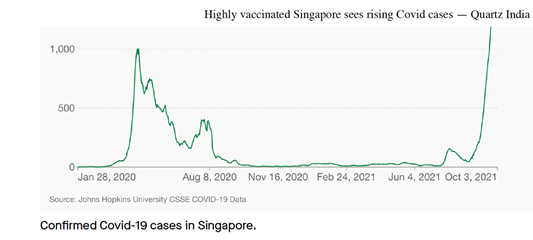
Omicron is spreading faster than previous variants of the novel coronavirus with the virus now in at least 90 countries since it first appeared in South Africa last month. Therefore, the Omicron variant could “out compete” other variants, including the more dangerous Delta variant – thus becoming the dominant variant. However, Omicron infections seem to be less severe and hospitalization and death nowhere near the rates of the other variants. Early reports suggest South Africa were reporting that people testing positive are presenting with mild symptoms: “In fact, they said, most of their infected patients were admitted for other reasons and have no Covid symptoms.” In other words, most of these patients had evidence of infection with SARS-CoV-2 but did not have COVID-19.[3]
What about Africa and Omicron?
There is something “mysterious” going on in Africa that is puzzling scientists, said Wafaa El-Sadr, chair of global health at Columbia University. “Africa doesn’t have the vaccines and the resources to fight COVID-19 that they have in Europe and the U.S., but somehow they seem to be doing better,” she said. Fewer than 6% of people in Africa are vaccinated.
“I think there’s a different cultural approach in Africa, where these countries have approached COVID-19 with a sense of humility because they’ve experienced things like Ebola, polio and malaria,” Sridhar said.

In past months, the coronavirus has pummeled South Africa and is estimated to have killed more than 89,000 people there, by far the most deaths on the continent. But for now, African authorities, while acknowledging that there could be gaps, are not reporting huge numbers of unexpected fatalities that might be COVID-19 related. WHO data shows that deaths in Africa make up just 3% of the global total. In comparison, deaths in the Americas and Europe account for 46% and 29%.
In Nigeria, Africa’s most populous country, the government has recorded nearly 3,000 deaths so far among its 200 million population. The U.S. records that many deaths every two or three days.[4]
Why Some Viruses Can Be Good
Not all viruses are bad, and perhaps the Omicron variant could actually help us to overcome the pandemic. Omicron, like some viruses, can actually fight against more dangerous viruses and more dangerous COVID-19 variants such as the Delta variant. Keep in mind that viruses typically evolve to become less lethal over time. Like wolves domesticated into dogs, disease-causing viruses seem to become tamer in an effort to survive. The reasoning goes that, sooner or later, SARS-CoV-2 must “lose its fangs and become as boring as the common cold”.[5]
Generally, like protective bacteria (probiotics), we have several protective viruses in our body. I am a believer in hormesis and building adaptive response/immunity. For example, viral infections at a young age are important to ensure the proper development of our immune system. Yet, we keep believing we should vaccinate against everything that poses a threat, even if the threat is mild. We should vaccinate when we have a real threat, and we have proven, non-leaky, and safe vaccines. But this should still be a personal decision and based on a multitude of factors; such as the frail and elderly. Elderly individuals are the most susceptible to an aggressive form of COVID-19, caused by SARS-CoV-2.
In some cases, latent (non-symptomatic) herpes viruses can help human natural killer cells (a specific type of white blood cell) identify cancer cells and cells infected by other pathogenic viruses. They arm the natural killer cells with antigens (a foreign substance that can cause an immune response in the body) that will enable them to identify tumor cells.[6]
Researchers working in Uganda said they found COVID-19 patients with high rates of exposure to malaria were less likely to suffer severe disease or death than people with little history of the disease.
If the Omicron variant is truly as transmissible as the say and significantly less harmful – some reports say 1/10 as strong – should we be afraid of it?
The main part of my personal practice is supporting people with cancer, and there are many situations where approaching cancer with low-dose metronomic chemotherapy yields significantly better results than standard-of-care high dose chemotherapy. In Oncology, systemic chemotherapies typically use the maximum tolerated dose to cause maximum tumor cell death. However, this paradigm has been challenged, particularly in older people and those who have reoccurring cancer, by theoretical models of tumor evolution, which suggest that removal of all cells that are sensitive to chemotherapy permits unopposed proliferation of any remaining resistant cells — a phenomenon called ‘competitive release’. Competitive release applies to viruses and different mutations and occurs when one of two species competing for the same resource disappears, thereby allowing the remaining competitor to utilize the resource more fully than it could in the presence of the first species.
Based on this model, an evolution-based treatment strategy that maintains a residual population of chemotherapy-sensitive cells should suppress growth of resistant cells when therapy is withdrawn, as the drug-sensitive cells have a fitness advantage in this condition.
A 2016 study designed an evolution-based treatment strategy using taxol (paclitaxel) adaptive therapy (AT), and compared this with standard taxol therapy (ST) in orthotopic xenograft mouse models of triple-negative and estrogen receptor-positive breast cancer. Two AT regimens were tested: AT-1, which maintains dosing frequency, but decreases paclitaxel dose as a tumor responds, and AT-2, which uses the same doses of paclitaxel, but doses are skipped when a tumor has responded. The treatment algorithms relied on tumor volume measurements determined by magnetic resonance imaging (MRI), as this could be used clinically.
In both mouse models, ST initially suppressed tumor growth, but exponential growth resumed following treatment cessation. AT-1 had the same effect as ST initially but was able to maintain a stable tumor burden similar to the initial tumor volume throughout the experiment (∼2 months). This allowed continued reduction of the paclitaxel dose, and eventually treatment withdrawal in some cases. Interestingly, AT-2 controlled tumor volume for longer than ST, but unlike AT-1, tumors treated using AT-2 eventually progressed. A direct comparison between AT-1 and AT-2 indicated that AT-1 provided better tumor growth control.[7]
The failure to trigger an effective adaptive immune response in combination with a higher pro-inflammatory tonus may explain why the elderly do not appropriately control viral replication and the potential clinical consequences triggered by a cytokine storm, endothelial injury, and disseminated organ injury.[8]

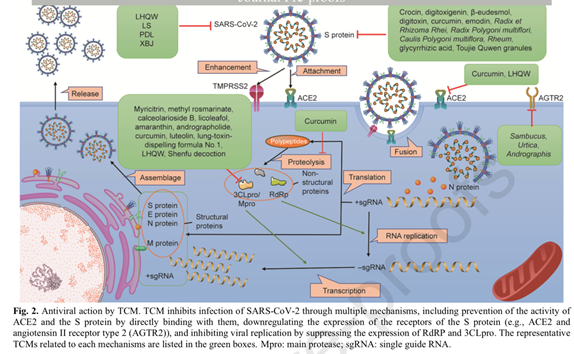
Perhaps the best approach would be to implement strategies, such as herbal medicine and nutritional compounds, including Zinc, Vitamin D, Quercetin, Selenium and an immune health-promoting diet, which provides a diverse and robust GUT microbiota. This would be a sensible, cost-effective, approach that supports and optimizes innate health and the immune response.
Dysregulation of the gut microbiota (gut dysbiosis) is an important risk factor as the gut microbiota is associated with the development and maintenance of an effective immune system response.[9] The elderly have a significantly increased susceptibility to infections and it has been reported that probiotic bacteria from the genus bifidobacterium can enhance certain aspects of cellular immunity in the elderly.[10] The best places to find this beneficial bacterium are yogurt, probiotics like kefir, or sauerkraut.
Selenium is a trace mineral which is deficient in many people. It plays an important role in free radical scavenging, targeting oxidative damage, a major factor in the COVID-19 “cytokine storm,” which is the immune response with an overproduction of cytokines and other immune cells that can lead to a rapid multi-organ failure and damage to the lungs, heart and kidneys.[11] Animal studies show that selenium with ginseng stem/leaf saponins increase the immune response against infectious bronchitis causes by a live coronavirus vaccine.[12]
This may provide all those infected by SARS-CoV-2, to develop a milder disease and help them to clear the virus through an efficient adaptive immune response. With a milder form of COVID-19, being infected by the Omicron variant could be the path to building natural immunity which builds effective immune memory that can persist for decades and typically results in enhanced responses and accelerated pathogen control, and a generation of robust and durable T and B cell alike;[13] and this goes beyond the detection of antibodies. The absence of specific antibodies in the serum does not necessarily mean an absence of immune memory.[14]
Wishing a Joyous Christmas, Winter Solstice, belated Chanukah, and a Happy New Year to you and our world. May our prayers be our words in deeds, and may our earth be made very peaceful because of each of us.
[1] https://www.medpagetoday.com/infectiousdisease/covid19/96309?xid=nl_covidupdate_2021-12-21&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=DailyUpdate_122121&utm_term=NL_Gen_Int_Daily_News_Update_active
[2] Lihong Liu, Sho Iketani, Yicheng Guo, Jasper Fuk Woo Chan, Maple Wang, Liyuan Liu, Yang Luo, Hin Chu, Yiming Huang, Manoj S. Nair, Jian Yu, Kenn Ka-Heng Chik, Terrence Tsz-Tai Yuen, Chaemin Yoon, Kelvin Kai-Wang To, Honglin Chen, Michael T. Yin, Magdalena E. Sobieszczyk, Yaoxing Huang, Harris H. Wang, Zizhang Sheng, Kwok-Yung Yuen, David D. Ho; Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, preprint doi: https://doi.org/10.1101/2021.12.14.472719
[3] Centers for Disease Control and Prevention, Glossary, Principles in Epidemiology in Public Health Practice, Third Edition, reviewed July 2, 2014, accessed December 17, 2021, https://www.cdc.gov/csels/dsepd/ss1978/glossary.html.
[4] MARIA CHENG and FARAI MUTSAKA, November 18, 2021·6 min read, Cheng reported from London. Rahim Faiez in Islamabad, Pakistan, and Chinedu Asadu in Lagos contributed to this report. https://sports.yahoo.com/why-double-mask-prevent-covid-235151606.html?utm_source=spotim&utm_medium=spotim_recirculation
[5] https://www.mcgill.ca/oss/article/covid-19/do-bad-viruses-always-become-good-guys-end, Jonathan Jarry M.Sc. | 18 Dec 2021, COVID-19, Do Bad Viruses Always Become Good Guys in the End?, McGill University
[6] https://theconversation.com/viruses-arent-all-nasty-some-can-actually-protect-our-health-117678, 08/2019, retrieved 12/16/2021
[7] Seton-Rogers, S. Preventing competitive release. Nat Rev Cancer 16, 199 (2016). https://doi.org/10.1038/nrc.2016.28
[8] Cunha LL, Perazzio SF, Azzi J, Cravedi P, Riella LV. Remodeling of the Immune Response With Aging: Immunosenescence and Its Potential Impact on COVID-19 Immune Response. Front Immunol. 2020 Aug 7;11:1748. doi: 10.3389/fimmu.2020.01748. PMID: 32849623; PMCID: PMC7427491.
[9] Chen J, Vitetta L, Henson JD, Hall S. The intestinal microbiota and improving the efficacy of COVID-19 vaccinations. J Funct Foods. 2021 Dec;87:104850. doi: 10.1016/j.jff.2021.104850. Epub 2021 Nov 10. PMID: 34777578; PMCID: PMC8578005.
[10] Chiang, B. L., Sheih, Y. H., Wang, L. H., Liao, C. K., & Gill, H. S. (2000). Enhancing immunity by dietary consumption of a probiotic lactic acid bacterium (Bifidobacterium lactis HN019): Optimization and definition of cellular immune responses. Eur J Clin Nutr. 2000 Nov;54(11):849-55
[11] Chen C, Zhang XR, Ju ZY, He WF. (2020). Advances In The Research Of Cytokine Storm Mechanism Induced By Corona Virus Disease 2019 And The Corresponding Immunotherapies. Zhonghua Shao Shang Za Shi (Chinese Journal of Burns), 36(0), E005. doi: 10.3760/cma.j.cn501120-20200224-00088. http://rs.yiigle.com/yufabiao/1183285.htm
[12] Ma X, Bi S, Wang Y, Chi X, Hu S. Combined Adjuvant Effect Of Ginseng Stem‐Leaf Saponins And Selenium On Immune Responses To A Live Bivalent Vaccine Of Newcastle Disease Virus And Infectious Bronchitis Virus In Chickens. Poult Sci. 2019;98:3548‐3556. https://doi.org/10.3382/ps/pez207
[13] Jarjour NN, Masopust D, Jameson SC. T Cell Memory: Understanding COVID-19. Immunity. 2021;54(1):14-18. doi:10.1016/j.immuni.2020.12.009
[14] Cox RJ, Brokstad KA. Not just antibodies: B cells and T cells mediate immunity to COVID-19. Nat Rev Immunol. 2020 Oct;20(10):581-582. doi: 10.1038/s41577-020-00436-4. PMID: 32839569; PMCID: PMC7443809.