I have always been a proponent of spending time outdoors in the fresh air, including the practice of forest bathing therapy for physical, mental, and spiritual wellbeing. Unfortunately, most people spend almost 90% of their time in indoor environments,[1] much to the detriment of their health.
At the onset of the pandemic, we were all told to stay inside and to avoid going outdoors. This seemed like a drastic and unhealthy recommendation to me, and I expressed my concerns about it at the time. For more than a year we were told to avoid outdoor activities unless we were wearing masks. In some places, people were not allowed to go outdoors except for essential errands. Even major parks and recreation trails in the remote areas were closed and people would wear masks outdoors when no one else was anywhere nearby. Fortunately, thinking has changed, and the general agreement among epidemiologists is that indoor transmission by airborne route is the greatest contributor to the spread of COVID-19, including super-spreader events.[2],[3],[4],[5]
Aerosol Inhalation is the Primary Way That COVID-19 Spreads
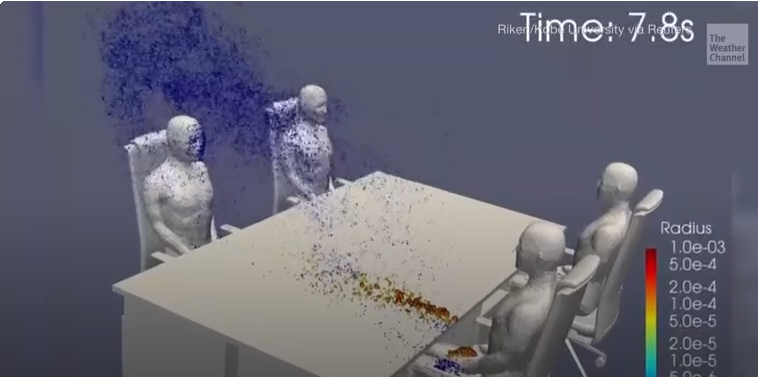
A growing body of epidemiological evidence indicates that the novel human coronavirus almost exclusively spreads from person-to-person via respiratory droplets or droplet nuclei. The risk of airborne SARS-CoV-2 infection transmission is highly dependent on both the duration of exposure and proximity to an infectious individual.

The CDC finally changed its guidance about the transmission of SARS-CoV-2, recognizing airborne spread as a key mode of infection. And the possibility of surface transmission, which frightened many people for months into using toxic chemicals for disinfection, has been deemed to be a rare occurrence.
The new guidance acknowledges that inhalation of aerosols—which are tiny, lightweight viral particles that can float and linger in the air for extended periods of time —is the primary way in which COVID-19 spreads. Even when an infectious person is more than 6 feet away, aerosols have the ability to travel and infect others.
Larger, heavier respiratory droplets can travel up to 6 feet, but then they fall to the ground. Smaller, aerosolized particles, however, can get caught in air flows and move throughout a space, infecting people at further distances.
Indoor Spaces with Poor Ventilation are Problematic
“It’s really the size of the droplet nuclei that defines an aerosol-borne infection versus a droplet-borne infection,” said Monica Gandhi, MD, MPH, an infectious disease expert at the University of California San Francisco. She added that in recognizing the airborne nature of COVID-19, we acknowledge that “it’s most effectively transmitted in closed, indoor spaces, and that ventilation is one of the most important things to mitigate the virus.” “Ventilation is emerging as one of the most important strategies to mitigate the pandemic,” she said.[6]
Current epidemiological evidence suggests that airborne SARS-CoV-2 infection transmission in confined, indoor spaces is plausible,[7] particularly when outdoor airflow rates are low. This means the “6-foot rule” which was widely promoted as providing safe social distancing doesn’t apply to closed indoor environments. From the beginning of the pandemic, I thought it was obvious that the same rules cannot apply for indoor and outdoor contact. The reality is that staying six feet apart outdoors is unnecessary, but six feet of social distancing indoors is likely not enough.[8]
In evaluating how the disease spreads, research shows that home-based outbreaks are the dominant category (79.9%), followed by transportation-based outbreaks (34.0%).[9] Many indoor spaces have a high occupant density, but do not provide adequate fresh air. This increases the infection risk through airborne transmission.[10]
According to the New York Times’s David Leonhardt, who spoke with multiple epidemiologists, “In truth, the share of transmission that has occurred outdoors seems to be below 1 percent and may be below 0.1 percent. The rare outdoor transmission that has happened almost all seems to have involved crowded places or close conversation.”
Dr. Pierre Kory from the FLCCC (Front Line COVID-19 Critical Care Alliance) states, “It is very difficult, if not nearly impossible, to give the virus to others outdoors via the airborne spread of tiny floating droplets because those droplets are, in most circumstances, quickly dispersed as a result of wind, air, or a person’s movement. Thus, the exhaled particle clouds get quickly diluted to the extent that there is not enough of a concentrated inoculum to infect others nearby. To date, there is only one true contact-traced, confirmed, documented outdoor transmission—and that was between two Chinese friends who spoke at close range for over an hour.” [11]
Closed Environments Facilitate Secondary Transmission
Research studies have attempted to identify common features of cases with COVID-19 so as to better understand what factors promote secondary transmission including superspreading events. In one Japanese study, a total of 110 cases were examined among eleven clusters and sporadic cases, with investigation of how the infections were transmitted.
Of the 110 cases examined, 27 (24.6%) were primary cases who generated 32 secondary cases. The odds that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment. The researchers concluded that it is plausible that closed environments contribute to secondary transmission of COVID-19 and promote superspreading events.[12]
In New York City, many nail salons have adopted the CDC’s guidelines for protecting employees and customers, such as practicing social distancing through a reduction in the capacity of services to fewer customers at any given time, removing waiting areas and accepting customers by appointment only, installing Plexiglas between service stations, and requiring all employees and customers to wear face masks at all times. Although all of these things may help a little, research shows that increased outdoor airflow is the number one way you can reduce the risk of airborne infection transmission.[13],[14]
Estimating the Effectiveness of Strategies for Reducing the Risk of SARS-CoV-2
Researchers have analyzed the effectiveness of various control strategies for reducing the risk of COVID-19. Here’s what they’ve found:
- Increased outdoor ventilation can reduce infection risk. An average of 27% reduction of infection risk can be achieved with 100% outdoor air (OA) for the ventilation system.
- A HEPA filter for recirculated air can offer an equivalent reduction. Doubling total supply airflow rate can reduce the infection risk by approximately 37% on average. Room air distributions can significantly impact the infection risk.
- Displacement ventilation can reduce the infection risk by 26%, while installing partitions can reduce more risk, around 46%. An average of 96% infection risk reduction can be achieved by integrating displacement ventilation and partitions.
- Personal ventilation can reduce the infection risk by 67%. The average risk reduction by air cleaners is around 31%, and the average reduction for the upper-room UVGI system is 59%.
- Wearing cloth masks can generally reduce considerable infection risk (average 48%).”[15]
My recommendation is to spend as much time outdoors as possible. If you cannot be outdoors, then be sure you have sufficient outdoor airflow. This is a critical precautionary measure when mitigating airborne infection transmission risk. Increased outdoor airflow has the potential to reduce the risk of airborne infection transmission to approximately <1% when face masks are worn by all occupants in a confined space.
Overall, I believe we need to have more free and open debate, which can actually empower society to proceed with educated policy decisions. This goes for Covid vaccinations as well. It must be established that vaccination is NOT mandatory, and we must ensure that no one is discriminated against for not having been vaccinated. Many do not want to be vaccinated because of possible health risks or concerns relating to long-term safety. In order to continue to minimize the risk of exposure and spread, we should all continue to take appropriate, reasonable precautions however, we can rest assured that being outdoors and in well ventilated environments is the safest place to be.
References
[1] Schweizer C., Edwards R.D., Bayer-Oglesby L., Gauderman W.J., Ilacqua V., Juhani Jantunen M., Lai H.K., Nieuwenhuijsen M., Künzli N. Indoor time–microenvironment–activity patterns in seven regions of Europe. J. Expo. Sci. Environ. Epidemiol. 2007;17:170–181. doi: 10.1038/sj.jes.7500490
[2] Shen J, Kong M, Dong B, Birnkrant MJ, Zhang J. A systematic approach to estimating the effectiveness of multi-scale IAQ strategies for reducing the risk of airborne infection of SARS-CoV-2 [published online ahead of print, 2021 Apr 30]. Build Environ. 2021;107926. doi:10.1016/j.buildenv.2021.107926
[3] Miller S.L., Nazaroff W.W., Jimenez J.L., Boerstra A., Buonanno G., Dancer S.J., Kurnitski J., Marr L.C., Morawska L., Noakes C. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. MedRxiv. 2020 doi: 10.1101/2020.06.15.20132027. 2020.06.15.20132027.
[4] Li Y., Qian H., Hang J., Chen X., Hong L., Liang P., Li J., Xiao S., Wei J., Liu L., Kang M. Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant. MedRxiv. 2020 doi: 10.1101/2020.04.16.20067728. 2020.04.16.20067728.
[5] Luo K., Lei Z., Hai Z., Xiao S., Rui J., Yang H., Jing X., Wang H., Xie Z., Luo P., Li W., Li Q., Tan H., Xu Z., Yang Y., Hu S., Chen T. Transmission of SARS-CoV-2 in public transportation vehicles: a case study in hunan province, China. Open Forum Infect. Dis. 2020;7 doi: 10.1093/ofid/ofaa430.
[6] D’Ambrosia, Amanda, Droplets vs Aerosols: What’s More Important in COVID-19 Spread? — CDC finally acknowledged aerosol transmission, but contribution to case counts remains unclear May 13th, 2021, https://www.medpagetoday.com/special reports/exclusives/92564?xid=nl_medpageexclusive_2021-05-13&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=MPTExclusives Winner_051321&utm_content=Final&utm_term=NL_Gen_Int_Medpage_Exclusives_Active
[7] Harrichandra A, Ierardi AM, Pavilonis B. An estimation of airborne SARS-CoV-2 infection transmission risk in New York City nail salons. Toxicol Ind Health. 2020 Sep;36(9):634-643. doi: 10.1177/0748233720964650. Epub 2020 Oct 21. PMID: 33085569; PMCID: PMC7578841.
[8] Centers for Disease Control and Prevention [CDC] (2020. c) Coronavirus disease 2019 (COVID-19): How it spreads, dated 16 June 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html (accessed 22 August 2020).
[9] Qian H., Miao T., Liu L., Zheng X., Luo D., Li Y. Indoor transmission of SARS‐CoV‐2. Indoor Air. 2020 doi: 10.1111/ina.12766. ina.12766
[10] Zhao L., Liu J. Operating behavior and corresponding performance of mechanical ventilation systems in Chinese residential buildings. Build. Environ. 2020;170:106600. doi: 10.1016/j.buildenv.2019.106600
[11] Kory, Pierre, Masks! – Clearing Up the Confusion, When to wear them, when not to wear them, that is the question. Jan 2, 2021, https://covid19criticalcare.com/guide-for-this-website/masks-clearing-up-the-confusion/
[12]Hiroshi Nishiura, Hitoshi Oshitani, Tetsuro Kobayashi, Tomoya Saito, Tomimasa Sunagawa, Tamano Matsui, Takaji Wakita, MHLW COVID-19 Response Team, Motoi Suzuki Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19), April 16, 2021, doi: https://doi.org/10.1101/2020.02.28.20029272
[13] Sun C, Zhai Z The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain Cities Soc. 2020 Nov; 62():102390.
[14] Amelia Harrichandra, A Michael Ierardi, Brian Pavilonis.,, An estimation of airborne SARS-CoV-2 infection transmission risk in New York City nail salons, Toxicol Ind Health. 2020 Sep; 36(9): 634–643. Published online 2020 Oct 21. doi: 10.1177/0748233720964650
[15] Shen J, Kong M, Dong B, Birnkrant MJ, Zhang J. A systematic approach to estimating the effectiveness of multi-scale IAQ strategies for reducing the risk of airborne infection of SARS-CoV-2 [published online ahead of print, 2021 Apr 30]. Build Environ. 2021;107926. doi:10.1016/j.buildenv.2021.107926

Very informative and useful set of guidance. With summer here, it will give everyone more opportunity to be outdoors. I have personally dropped putting on a mask during my morning walk. The mask stays in my pocket so I can use it if I do get close to someone!