Although statistics show that people over the age of 65 have an increased risk of contracting COVID-19 and dying from complications due to underlying conditions, it appears that it has more to do with nutritional status than age alone. It’s true that the older we get, the more nutritional deficiencies we may have, primarily because of poor dietary choices throughout life.
Unfortunately, nutrition is often overlooked in favor of pharmaceuticals and other medical interventions. But diet plays a critical role in fortifying the immune system and in helping the body fight off and overcome infections such as COVID-19.
The Foundation of a Healthy Immune System
Often missing in public health discussions around immunity and infection are nutritional strategies to encourage optimal function of the immune system. In spite of the long history and tradition of botanical medicine—supported by a large body of scientific data—herbs are rarely mentioned as useful allies for enhancing immune function.
I find it surprising that nutrition is rarely mentioned for its role in immune function. The importance that nutrition plays in immune function is well established, and tends to be predictable and linear. This should make nutritional recommendations appealing and accessible to the allopathically-trained mind. Botanical medicine, however, is more complex, because each single plant has a multitude of active compounds. The application becomes even more intricate when several botanicals are combined. Because allopathic medicine tends to focus on a ‘magic bullet’ cure, I believe this complexity makes it more of a stretch for conventional doctors to embrace botanical medicine.
There seems to be a great deal of extreme bias and fear when it comes to botanical, nutritional, and even dietary means to help support our well-being. Meanwhile, every day there is a published scientific paper on the benefits of specific nutrients and herbs in combating COVID-19, but I have yet to see these studies mentioned in the media.

The same cautions are repeated constantly: Wear a mask, practice social distancing, and wash your hands (we now have an epidemic of eczema as a result[1]) while we wait for a vaccine that is safe for everyone and will put a halt to the pandemic.
Protective Nutrients for Immune Health
Many key nutrients—including vitamins A, B6, B12, C, D, E, and folate;=, and trace elements, including zinc, iron, selenium, magnesium, and copper, play important and complementary roles in supporting both the innate and adaptive immune systems. Vital information on the role of these nutrients in our society garners little attention and tends to go unnoticed, despite the widespread deficiencies in our society, especially among the elderly, who are most at risk for severe outcomes associated with viral infections. In addition, suboptimal status in micronutrients negatively affects immune function and can decrease resistance to infections.
In the case of COVID-19, nutrient deficiencies increase the risk of complications, including the inflammatory cytokine storm. Few studies have been done on the effect of dietary components on prevention of COVID-19, however, a recent systematic review concluded that supplementation with many of these nutrients may be effective in improving the health status of patients with viral infections.[2]
The Importance of Vitamin D and Zinc in Immunity
Two of the most essential nutrients for immune health are vitamin D and zinc. Vitamin D profoundly influences immunity, and a deficiency clearly increases the risk for respiratory infections. Many immune cells have vitamin D receptors that affect their function after ligand binding. A recent research review article highlighted the current status of vitamin D deficiency, the mechanisms of action of vitamin D and the current literature on the topic, with a special focus on the potential implications for the COVID-19 pandemic.[3]

A growing body of circumstantial evidence now specifically links outcomes of COVID-19 and vitamin D status.[4] Several recent studies have concluded that low levels of vitamin D are associated with increased risk of COVID-19 and/or severity of COVID-19 infections.3,4,[5],[6],7,8
A univariate analysis demonstrated an association between low plasma 25(OH)D level and increased likelihood of COVID‐19 infection and of hospitalization due to the SARS‐CoV‐2 virus.[7]
In a cross-sectional analysis across Europe, COVID-19 mortality was significantly associated with vitamin D status in different populations.[8]
Even marginal zinc deficiency can negatively affect immunity. Zinc is important for the maintenance and development of cells in both the innate and adaptive immune systems. A deficiency results in impaired formation, activation and maturation of lymphocytes, disturbs the intercellular communication via cytokines, and weakens the innate host defense.
Research studies suggest that zinc could have protective effects against COVID-19 by supporting anti-viral immunity and reducing inflammation. A team of researchers in Moscow, Russia, led the review and published it in the International Journal of Molecular Medicine.
“According to the current estimates, the risk of zinc deficiency is observed in more than 1.5 billion people in the world,” explains lead author of the review Prof. Anatoly Skalny, who heads the Laboratory of Molecular Dietetics at Sechenov University.[9] One study showed that zinc blocks the enzyme responsible for replicating the coronavirus that led to the SARS outbreak of 2002.[10]
Essential Fatty Acids and Inflammation
An inflammatory cascade (or ‘cytokine storm’) triggered by COVID-19 is one of the most dangerous aspects of the disease. It makes sense to consider dietary protocols that help the body naturally regulate inflammation.
Essential fatty acids have long been recognized for their role in calming inflammation. In particular, nutritional deficiencies in the essential fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) result in delayed or suboptimal resolution of inflammation.[11]
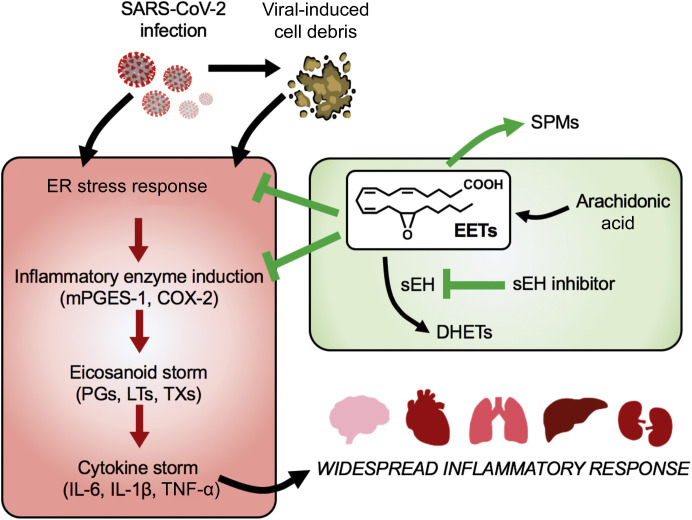
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection leads to severe tissue damage, which releases cell debris.
Research shows that omega-3 fatty acid–derived EPA and DHA exhibit anti-inflammatory activity in various inflammatory diseases, including in the lung, heart, ocular angiogenesis, and pain.[12]
EPA and DHA help reduce inflammation during sepsis, a leading cause of death from infections. In one study, an enteral (tube feeding) diet enriched with EPA + GLA (borage oil) + antioxidants for 28 days was administered to patients with severe sepsis or septic shock who needed mechanical ventilation. The authors observed that the diet enriched with EPA and DHA contributed to improved clinical outcomes in the ICU individuals and that the treated group presented lower mortality rates when compared to the control group.[13]
More recently, a Cochrane review showed that patients with acute respiratory distress syndrome (ARDS) receiving EPA and DHA supplementation showed a significant improvement in blood oxygenation and reduction in ventilation requirement, organ failures, length of stay in the ICU and mortality at 28 days.[14]
Thus, supplementation with EPA and DHA could have important implications in critically ill COVID-19 patients. It should also be noted that optimal nutritional support for the immune system often requires intakes above the RDA for some micronutrients, while at the same time infections and other stressors can reduce micronutrient status in the body.[15]
N-acetylcysteine (NAC) Blocks Inflammatory Cascade
N-acetylcysteine (NAC) has always been one of my favorite supplements. In a severe COVID-19 infection, it has been shown to induce a therapeutic blockade of inflammation. NAC is a potent redox-antioxidant that has been used clinically to treat a wide variety of medical issues and conditions, including paracetamol overdose, acute respiratory distress syndrome, chemotherapy, and heavy metal-induced toxicity. It is also used as a mucolytic agent and to ameliorate certain psychiatric disorders.[16],[17] Furthermore, NAC has been reported to have multiple other beneficial properties, such as enhancing bone regeneration, reducing tinnitus, easing post surgical complications and providing protective effects during mutagenic irradiation.[18]
Studies show that NAC is effective at reducing acute attacks of chronic bronchitis. A meta-analysis from 2000 looked at 8 different studies and concluded that NAC prevented acute exacerbations of chronic bronchitis.[19] Another systematic review published in the same year showed similar results, finding that NAC significantly reduced the symptoms of chronic bronchitis compared to a placebo.[20]
Administration of NAC during the winter months appears to significantly reduce influenza and influenza-like episodes, especially in elderly high-risk individuals. [21]
With COVID-19 infections, glucose 6-phosphate dehydrogenase (G6PD) deficiency facilitates human coronavirus infection due to glutathione depletion. G6PD deficiency may especially predispose to hemolysis (destruction of red blood cells) upon COVID-19 infection when employing pro-oxidant therapy. However, glutathione depletion is reversible by N-acetylcysteine (NAC) administration.
A severe case of COVID-19 infection in a G6PD-deficient patient treated with NAC benefited from intravenous (IV) NAC beyond the reversal of hemolysis. NAC blocked hemolysis and elevation of liver enzymes, C-reactive protein (CRP), and ferritin and allowed removal from respirator and veno-venous extracorporeal membrane oxygenator. The G6PD-deficient patient made full recovery. NAC was also administered to 9 additional respirator-dependent COVID-19-infected patients without G6PD deficiency. NAC elicited clinical improvement and markedly reduced CRP in all patients and ferritin in 9 of 10 patients.
NAC mechanism of action may involve the blockade of viral infection and the ensuing cytokine storm, as illustrated below:
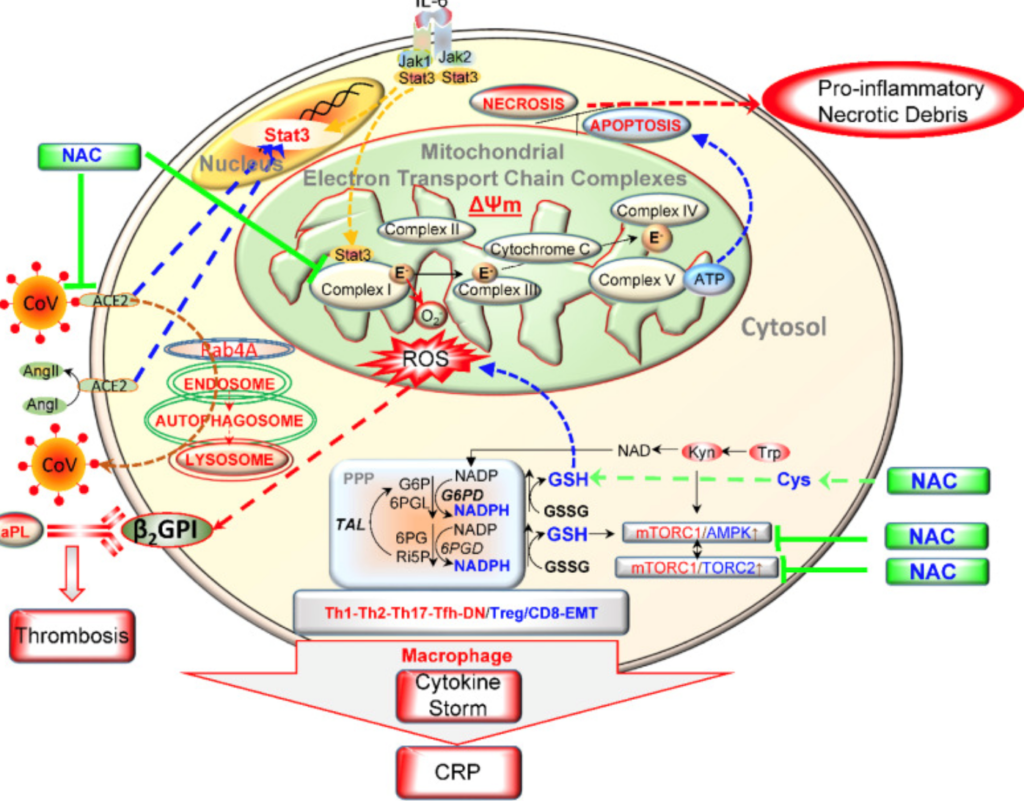
Since one of the main symptoms of COVID-19 is a cough, it’s possible that NAC could help to reduce the severity of this symptom. It seems to help in a variety of lung disorders by affecting glutathione and reducing inflammation.[23]
Using Nutrition to Improve Outcome in COVID-19
There is no question that a healthy diet is fundamental to maintaining well-being and decreasing the risk of disease. Foodomics is a new approach to food and nutrition that studies the food domain as a whole to attain the main objective, which is the optimization of human health and well-being.[24] I firmly believe that supporting and improving overall health and nutritional status could significantly improve outcomes in COVID-19 as well as other diseases.
Zinc Rich Foods Photo courtesy of VAYA
https://vaya.in/news/foods-rich-in-zinc-and-vitamin-d/
[1] Pradhan S, Kroumpouzos G, Goldust M. Hand eczema due to frequent hand washing in combat with COVID-19 [published online ahead of print, 2020 Jul 27]. J Cosmet Dermatol. 2020;10.1111/jocd.13639. doi:10.1111/jocd.13639
[2] BourBour F, Mirzaei Dahka S, Gholamalizadeh M, et al. Nutrients in prevention, treatment, and management of viral infections; special focus on Coronavirus [published online ahead of print, 2020 Jul 9]. Arch Physiol Biochem. 2020;1-10. doi:10.1080/13813455.2020.1791188
[3] Verdoia M, De Luca G. Potential role of hypovitaminosis D and Vitamin D supplementation during COVID-19 pandemic [published online ahead of print, 2020 Jul 31]. QJM. 2020;hcaa234. doi:10.1093/qjmed/hcaa234
[4] Mitchell F. Vitamin-D and COVID-19: do deficient risk a poorer outcome?. Lancet Diabetes Endocrinol. 2020;8(7):570. doi:10.1016/S2213-8587(20)30183-2
[5] Verdoia M, De Luca G. Potential role of hypovitaminosis D and Vitamin D supplementation during COVID-19 pandemic [published online ahead of print, 2020 Jul 31]. QJM. 2020;hcaa234. doi:10.1093/qjmed/hcaa234
[6] Mitchell F. Vitamin-D and COVID-19: do deficient risk a poorer outcome?. Lancet Diabetes Endocrinol. 2020;8(7):570. doi:10.1016/S2213-8587(20)30183-2
[7] Merzon E, Tworowski D, Gorohovski A, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study [published online ahead of print, 2020 Jul 23]. FEBS J. 2020;10.1111/febs.15495. doi:10.1111/febs.15495
[8] Laird, E., Rhodes, J., Kenny RA., Vitamin D and Inflammation: Potential Implications for the Severity of COVID-19, Irish Medical Journal, Vo. 113, No. 5, P 81, http://imj.ie/vitamin-d-and-inflammation-potential-implications-for-severity-of-covid-19/, Aust. 11, 2020
[9] Skalny AV, Rink L, Ajsuvakova OP, Aschner M, Gritsenko VA, Alekseenko S , Svistunov AA, Petrakis D, Spandidos DA, Aaseth J, Aaseth J, et al: Zinc and respiratory tract infections: Perspectives for COVID‑19 (Review). Int J Mol Med 46: 17-26, 2020
https://www.medicalnewstoday.com/articles/zinc-may-have-protective-effects-against-covid-19#Zinc-and-the-immune-system, retrieved July 21, 2020
[10] Aartjan J. W. te Velthuis, Sjoerd H. E. van den Worm, et. al., Zn2+ Inhibits Coronavirus and Arterivirus RNA Polymerase Activity In Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture, Published: November 4, 2010, https://doi.org/10.1371/journal.ppat.1001176
[11] Hammock BD, Wang W, Gilligan MM, Panigrahy D. Eicosanoids: The Overlooked Storm in Coronavirus Disease 2019 (COVID-19)? [published online ahead of print, 2020 Jul 8]. Am J Pathol. 2020;S0002-9440(20)30332-1. doi:10.1016/j.ajpath.2020.06.010
[12] Schunck W.H., Konkel A., Fischer R., Weylandt K.H. Therapeutic potential of omega-3 fatty acid-derived epoxyeicosanoids in cardiovascular and inflammatory diseases. Pharmacol Ther. 2018;183:177–204.
[13] Pontes-Arruda A., Aragão A.M.A., Albuquerque J.D. Effects of enteral feeding with eicosapentaenoic acid, γ-linolenic acid, and antioxidants in mechanically ventilated patients with severe sepsis and septic shock. Crit. Care Med. 2006;34:2325‐2333. https://doi: 10.1097/01.CCM.0000234033.65657.B6
[14] Dushianthan A., Cusack R., Burgess V.A., Grocott M.P., Calder P.C. Immunonutrition for acute respiratory distress syndrome (ARDS) in adults. Cochrane Database Syst. Rev. 2019;1:CD012041. doi: 10.1002/14651858.CD012041.pub2.
[15] Calder, PC. Anitra AC., Gombart, AF., Eggersdorfer M., Optimal Nutritional Status for aWell-Functioning Immune System Is an Important Factor to Protect against Viral Infections Nutrients 2020, 12, 1181; doi:10.3390/nu12041181
[16] Samuni Y, Goldstein S, Dean OM, Berk M. The chemistry and biological activities of N-acetylcysteine.
Biochim Biophys Acta. 2013 Aug; 1830(8):4117-29.
[17] Chen MJ, Wang HY, Chang CW, Hu KC, Hung CY, Chen CJ, Shih SC. The add-on N-acetylcysteine is more effective than dimethicone alone to eliminate mucus during narrow-band imaging endoscopy: a double-blind, randomized controlled trial. Scand J Gastroenterol. 2013 Feb; 48(2):241-5.
[18] Gao X, Lampraki EM, Al-Khalidi S, Qureshi MA, Desai R, Wilson JB. N-acetylcysteine (NAC) ameliorates Epstein-Barr virus latent membrane protein 1 induced chronic inflammation. PLoS One. 2017;12(12):e0189167. Published 2017 Dec 11. doi:10.1371/journal.pone.0189167
[19] Vida Mokhtari, M.Sc.1, 2, 3, Parvaneh Afsharian, Ph.D.2, Maryam Shahhoseini, Ph.D.2, Seyed Mehdi Kalantar, Ph.D.1, Ashraf Moini, M.D. A Review on Various Uses of N-Acetyl Cysteine, CELL JOURNAL(Yakhteh), Vol 19, No 1, Apr- Jun (Spring) 2017
[20] Stey, C., Steurer, J., Bachmann, S., Medici, T., & Tramer, M. (2000). The effect of oral N-acetylcysteine in chronic bronchitis: a quantitative systematic review. European Respiratory Journal, 16:253-62.
[21] S. De Flora*, C. Grassi**, L. Carati Attenuation of influenza-like symptomatology and improvement of cell-mediated immunity with long-term N-acetylcysteine treatment, Eur Respir J 1997; 10: 1535–1541 DOI: 10.1183/09031936.97.10071535
[22] Ibrahim H, Perl A, Smith D, et al. Therapeutic blockade of inflammation in severe COVID-19 infection with intravenous n-acetylcysteine [published online ahead of print, 2020 Jul 21]. Clin Immunol. 2020;108544. doi:10.1016/j.clim.2020.108544
[23] Tiouvanziam, R., Conrad, C., Bottiglieri, T., Herzenberg, L., et al. (2006). High-dose oral N-acetylcysteine, a glutathione prodrug, modulates inflammation in cystic fibrosis. Proceedings of the National Academy of Sciences of the United States of America, 103(12):4628-33.
[24] Capozzi F, Bordoni A. Foodomics: a new comprehensive approach to food and nutrition. Genes Nutr. 2013;8(1):1-4. doi:10.1007/s12263-012-0310-x

Thanks Donnie. I so appreciate your insights. Question, can you get NAC by eating certain foods?
Donnie
I came to see you many years ago as I could not take estrogen through menopause as my Breast cancer history is strong. You are a miracle worker and got me through those awful years. You were in Norwalk at that time. Wonderful to hear of your continued success since your move.
A few years ago I read a headline on a gent who was on a program successfully for prostate cancer. I KNEW BEFORE READING ON THAT YOU WERE HIS “MIRACLE WORKER”
Continued success, be safe and be BLESSED.
PS please keep forwarding this Information. Most helpful