As we transition into fall and winter and COVID-19 infections and hospitalizations rise dramatically, it’s clear that the virus isn’t going away any time soon. Although the promise of a vaccine is on the horizon, there’s no certainty as to its long-term effectiveness and many are concerned about the safety of its contents.
I continue to find compelling information that supports the use of natural medicines such as medicinal mushrooms, elderberry, and vitamin D against infections, as well as new facts and insights into how COVID-19 spreads and what populations are most vulnerable and why. All of this supports my belief that there is a great deal we can do to obtain robust health and build our immunological defense against pathogens, and thereby significantly reduce our risk of contracting the virus and the dreaded complications associated with it.
Supporting the Lungs and a Healthy Inflammatory Response Function with Immunomodulating Compounds from Medicinal Mushrooms
One of the aspects of COVID-19 that poses a dangerous threat is the acute inflammation triggered by the virus. A number of medicinal mushrooms and herbs have potent anti-viral and anti-inflammatory activity, making them promising candidates for effective treatments. Research indicates that medicinal mushroom extracts could have prophylactic or therapeutic effects against the pneumonic superinfection and severe lung inflammation that often complicates COVID-19 infection.[1]
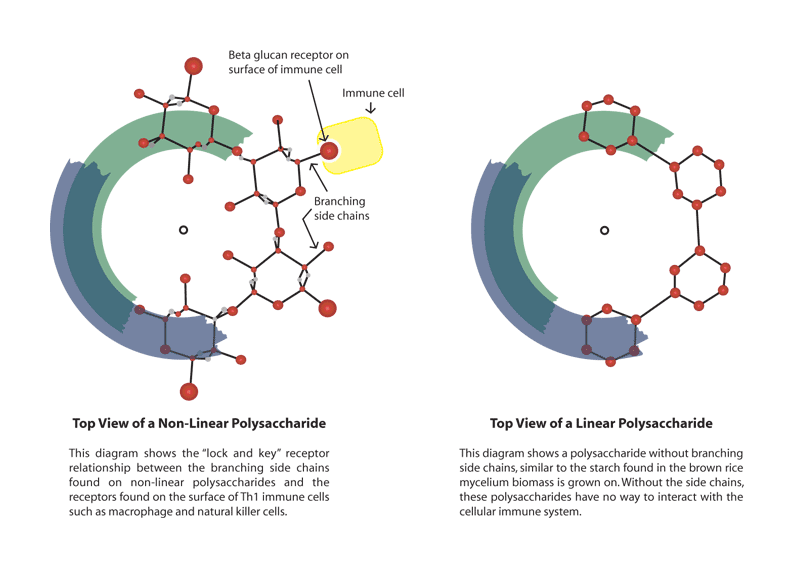
β‐glucans (a group of polysaccharides) constitute the main part of the cell wall in fungi and are potent immunomodulators. These compounds have been investigated in clinical studies including Reishi / Lingzhi mushroom (Ganoderma lucidum) and Turkey Tail mushroom (Trametes versicolor / Coriolus versicolor) (PSK and PSP), as well as lentinan from Shiitake mushroom (Lentinula edodes).[2]
Beta-glucans stimulate macrophages to produce cytokines (local immunomodulators) and these in turn activate adaptive immunity against foreign antigens, which involves both B and T cells. B cells produce antibodies to mediate humoral immunity, whereas T cells induce cell-mediated immunity.[3]
β‐glucans have been shown to be effective against cancer and infections.[4],[5],[6],[7] They have also been shown to improve quality of life and overall survival in patients undergoing chemotherapy or radiation treatment.[8]
Researchers hypothesize that β-glucans derived from medicinal mushrooms have the potential to alleviate the immune cascade in pathological conditions such as ARDS that is experienced by COVID-19 patients.
Let’s take a closer look at some of these medicinal mushrooms.
Shiitake Mushrooms (Lentinula edodes)
Studies show that β-glucan rich lentinan extract demonstrates in vitro immunomodulatory and pulmonary cytoprotective effects. These effects may have positive relevance to COVID-19 therapeutics targeting the cytokine storm that is such a dangerous aspect of the virus.
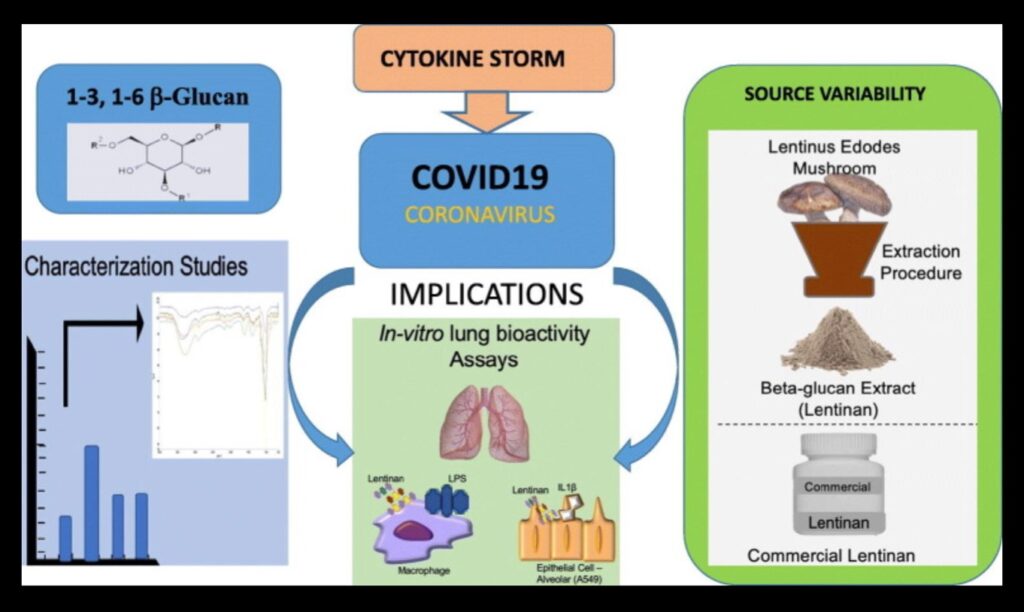
In research, β-glucan rich Lentinus edodes demonstrated potential for the treatment of lung injury. When compared to a commercial source of the same mushroom, the lentinan extract containing higher levels of β-glucan and lower levels of α-glucan was significantly more effective. [9] This points to the utmost importance of the quality of the mushroom extract. It’s important to realize that most commercial mushroom extracts are of poor quality.[10]
Cordyceps Mushroom (Cordyceps militaris)
The multiple pharmacological activities of cordyceps have attracted the attention of researchers. Cordycepin is the major bioactive component extracted from the medicinal mushroom Cordyceps militaris.
Results from a recent review indicate that cordycepin exerts protective effects against inflammatory injury for many diseases including acute lung injury, asthma, rheumatoid arthritis, Parkinson’s disease, hepatitis, atherosclerosis, and atopic dermatitis. Cordycepin enhanced immunity inhibited the proliferation of viral RNA and suppressed cytokine storms. Cordycepin and its analogs show great promise as the next new class of anti-inflammatory agents.[11]
Chaga Mushroon (Inonotus obliquus)
Chaga relieves nasopharyngeal inflammation and has been widely used in traditional medicine to improve respiratory function in Asia and some European countries. Extracts from this fungus have been used for its anti-oxidant, hepato-protective and anti-inflammatory properties.[12]
Shatavari (Asparagus racemosus)
Shatavari is frequently recommended in Ayurvedic medicine for reproductive health disorders in women and as a major health tonic. A recent investigational study identified compounds from Asparagus racemosus against SARS-CoV-2 using molecular docking and dynamics studies.
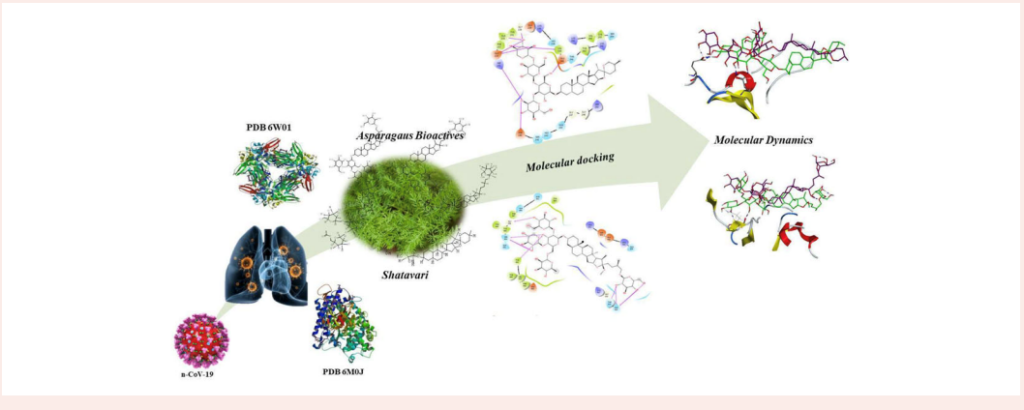
According to the study, phytochemicals in Shatavari showed promising in-silico docking and molecular dynamics, and Asparaoside-C and Asparoside-F exhibited good binding with target proteins. The researchers concluded that Asparagus racemosus holds promise as a SARS-COV-2 (S) and (N) proteins inhibitor.[13]
Recent Research into Elderberry Demonstrates Promise for Managing Covid-19
I first wrote extensively about the benefits of elderberry (Sambucus nigra) at the beginning of the pandemic. Since that time, evidence obtained from a review of five clinical studies involving 936 adults indicates that herbal preparations of elderberry, when taken within 48 hours of onset of acute respiratory viral infection, may reduce the duration and severity of common cold and influenza symptoms. The researchers therefore suggest further studies into the effectiveness of elderberry for the treatment of COVID-19 based on the following findings:
- Mono-herbal preparations of elderberry (in extract or lozenge formulation) may reduce influenza-type symptoms, including fever, headache, nasal congestion and nasal mucous discharge, when taken within the first 48 hours of symptom onset.
- Within 2–4 days of elderberry treatment, most participants experienced significant symptom reduction. With 4 days of elderberry treatment, most participants experienced significant symptom reduction, by an average of 50 %.[14]
Vitamin D Deficiency Associated with Increased Risk of Covid-19 Susceptibility and Severity
Adequate serum levels of vitamin D have been shown to affect the severity of COVID-19 infections. In a case-controlled study in China comparing serum 25(OH)D levels and rates of vitamin D deficiency (VDD) between 80 healthy controls and 62 patients diagnosed with COVID-19, cases were categorized into asymptomatic, mild/moderate, and severe/critical disease. Logistic regression analysis was conducted to examine the associations between 25(OH)D level, or VDD, and case status/severity of COVID-19 while controlling for demographics and comorbidities. A threshold level of vitamin D for conveying COVID-19 risk was estimated.
Those with severe/critical COVID-19 cases were significantly older and had higher percentages of comorbidity (renal failure) compared to mild cases. Testing showed that the serum 25(OH)D concentration in COVID-19 patients was much lower than that in healthy controls. And 25(OH)D level was the lowest in severe/critical cases, compared with mild cases. Researchers concluded that elderly and people with comorbidities were susceptible to severe COVID-19 infection. VDD was a risk factor for COVID-19, especially for severe/critical cases.[15]
Bisphenol A (BPA) and the Risk for SARS-CoV-2 Infection and Severe COVID-19
The risk of severe COVID-19 is increased by certain underlying comorbidities, including asthma, cancer, cardiovascular disease, hypertension, diabetes, and obesity. Exposure to hormonally active chemicals called endocrine-disrupting chemicals (EDCs) can promote cardio-metabolic diseases, endocrine-related cancers, and immune system dysregulation and may be linked to higher risk of severe COVID-19.
Bisphenol ABPA is among the most common EDCs and exerts its effects via receptors that are widely distributed in human tissues, including nuclear estrogen receptors (ERα and ERβ). BPA exposure appears to increase the effects on key SARS-CoV-2 infection mediators, such as angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2. The potential role of BPA on the risk and severity of COVID-19 merits further investigation.[16]
The Truth About Aerosols and COVID-19 Spread
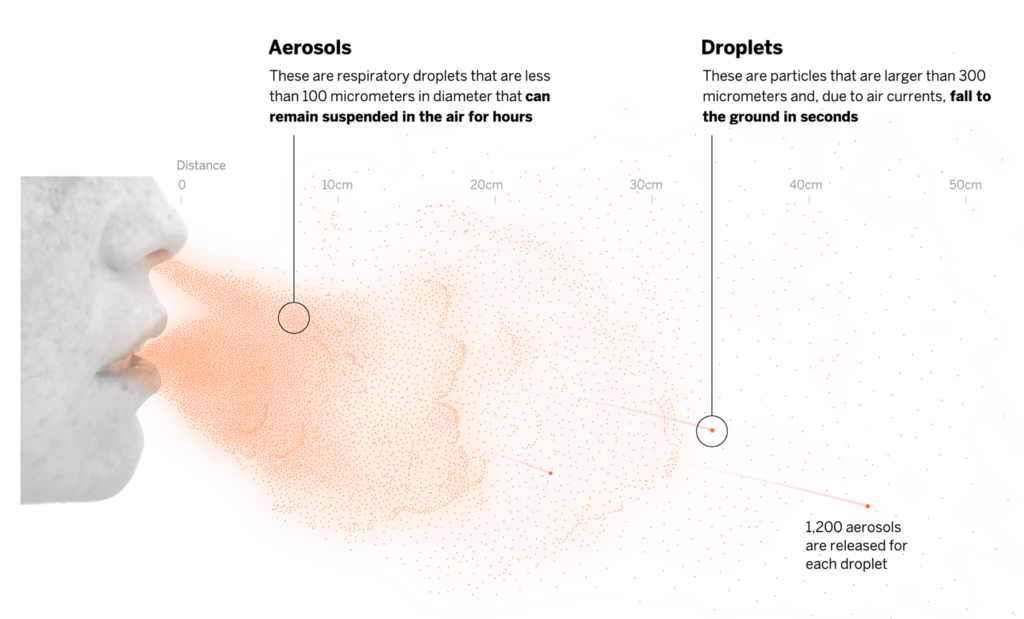
Compelling evidence indicates that COVID-19 transmission via small-particle aerosols, not droplets, is the primary way that the virus spreads. Researchers from the American Association for Aerosol Research suggest that the World Health Organization (WHO) and the CDC have been reluctant to embrace aerosol transmission in part due to ‘historical bias,’ despite significant evidence of aerosol transmission.
Linsey Marr, PhD, of Virginia Tech University, noted the CDC’s recent acknowledgement that SARS-CoV-2 can “sometimes” be spread through aerosols, though she crossed out the word “sometimes” to write “commonly.”
“The definitions are still resting on epidemiology, but it doesn’t really reflect what we understand about mechanisms” of transmission, she said. “Understanding mechanisms is important [for] how we can best apply interventions and slow this down.”
As evidence of historical bias, Jose-Luis Jimenez, PhD, of the University of Colorado in Boulder, cited research from as recently as 1985 about measles. At that time, measles was thought to be spread by large respiratory droplets and close contact. Now, we know that airborne aerosols spread the measles virus.
Jimenez argued there is more evidence for aerosol spread of COVID-19 than via droplets, and noted there is no evidence for droplets in super-spreading events, impact of reduced ventilation, or transmission by asymptomatic people without a cough.
As an example, Jimenez pointed to the case study of the COVID-19 super-spreading event from the choir practice in Skagit County, Washington. In that event, a two-and-a-half hour rehearsal with one index case of COVID-19 produced 52 new infections, with some people some standing more than 42 feet away. He ruled out fomites (surfaces that may have been contaminated), not only because are they inefficient for SARS-CoV-2 transmission, according to the CDC, but the index case didn’t touch any objects. Jimenez also ruled out droplets, because the index case “didn’t talk to others,” and there was no way to impact droplets on eyes, nostrils, and mouths of 52 people.
However—the choir room had poor ventilation, and people were there for an extended period of time, singing and talking, and with no masks. All of this points to aerosol spread, said Jimenez.
Marr emphasized the importance of poor ventilation and crowded spaces in facilitating COVID-19 spread. She discussed Japan’s “3 Cs” for infection control that the country’s government emphasized during the COVID-19 pandemic: closed spaces with poor ventilation, close contact settings, and crowded spaces.
While facemasks help prevent both aerosol and droplet transmission, Marr sounded a note of caution about face shields as a substitute for masks. She acknowledged that face shields are effective for large droplets that might land on eyes, nose, or mouth, but noted that they are ineffective against aerosols.
Jimenez stressed that given the risk of aerosol transmission, wearing a mask is essential, even if people are rigorous about maintaining social distance. He also emphasized the importance of increasing ventilation and using air filtration. Marrs concurs, stating that if a place “feels stuffy or you smell things,” that is an indication that ventilation is insufficient.[17]
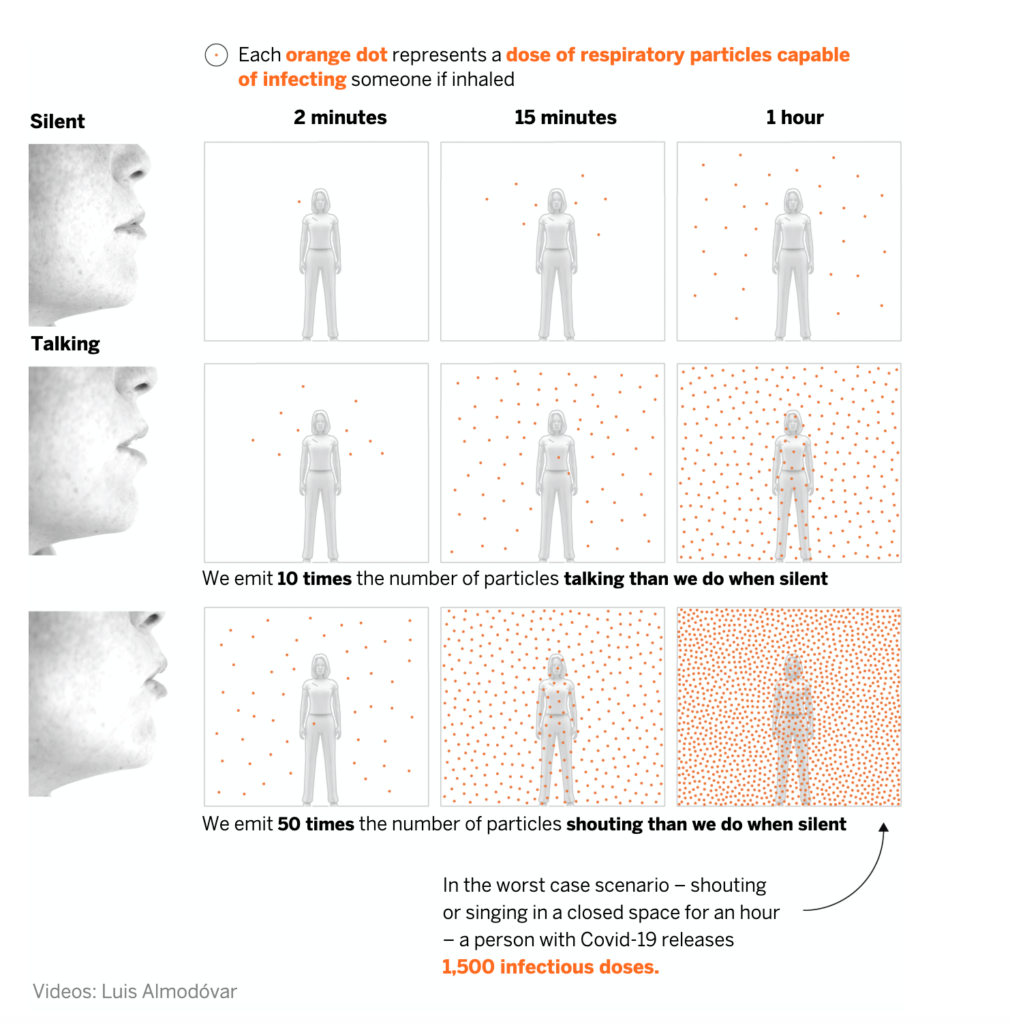
How the Coronavirus is Spread Through the Air and How to Reduce Risk
The risk of contagion is highest in indoor spaces but can be reduced by applying all available measures to combat infection via aerosols. Here is an overview of the likelihood of infection in three everyday scenarios, based on the safety measures used and the length of exposure.
Blood Type and The Risk and Severity of COVID-19
Scientists have noted that blood type O seems to be associated with a reduced risk of developing COVID-19 and the severity of the disease.

Two retrospective studies support these observations.
In Denmark, recent research indicates a lower-than-expected prevalence of blood group O individuals among COVID-19 patients. In addition, researchers note that blood groups are “increasingly recognized to influence susceptibility to certain viruses,” among them SARS-CoV-1 and norovirus. Individuals with A, B, and AB blood types may be at increased risk for thrombosis and cardiovascular diseases, which are significant comorbidities among patients hospitalized with COVID-19.
Among individuals testing positive for SARS-CoV-2, about 38% belonged to blood group O versus about 42% of those in the reference population. There were significantly more group A and AB individuals in the positive testing group versus the reference population, though the difference was non-significant for group B. When group O individuals were removed, there was no difference between the remaining groups.[18]
A second study from the University of British Columbia in Vancouver reported a connection between blood type and COVID-19 severity. Blood types A or AB in COVID-19 patients were associated with increased risk for mechanical ventilation, continuous renal replacement therapy, and prolonged ICU admission versus patients with blood type O or B. Inflammatory cytokines did not differ between groups, however.
There was no difference in probability of ICU discharge, and eight patients died in the O/B group versus nine patients in the A/AB group. Biomarkers of renal and hepatic dysfunction were higher in the A/AB group, as well. “The unique part of our study is our focus on the severity effect of blood type on COVID-19. We observed this lung and kidney damage, and in future studies, we will want to tease out the effect of blood group and COVID-19 on other vital organs,” noted the researchers.[19]
“The largest dataset of COVID patients is in the Medicare dataset recently did the largest study of COVID outcomes to date, and that is about half a million Medicare beneficiaries with the confirmed diagnosis code after April 1st right up until April 31st. Of those half a million cases, we also studied 38,000 inpatient deaths.
Harlan Krumholz, MD, of Yale University recently laid out these facts regarding Covid-19:
- “Hispanic patients were at the highest risk in terms of the race with the highest risk, at 74% increased risk of mortality after adjusting for comorbidities.
- We (USA) have the most comorbid country, probably, in the world, in the most contemporary time in the world.
- We have the most obese,
- the most comorbid,
- the most hospitalized,
- the most medicated,
- the most disabled population in the history of the world.”[20]
I’m sure it comes as no surprise that I believe our best approach to the threat of the virus is to strengthen our overall health and vitality, while bolstering our body’s natural defenses. Natural approaches hold great appeal because they are safe and readily available to all of us. May you continue to find ways to be your healthiest self and stay well during these challenging times.
[1] Hetland G, Johnson E, Bernardshaw SV, Grinde B. Can medicinal mushrooms have prophylactic or therapeutic effect against COVID-19 and its pneumonic superinfection and complicating inflammation? Scand J Immunol. 2020 Jul 13:e12937. doi: 10.1111/sji.12937. Epub ahead of print. PMID: 32657436; PMCID: PMC7404338.
[2] Pan P, Huang YW, Oshima K, et al. The immunomodulatory potential of natural compounds in tumor-bearing mice and humans. Crit Rev Food Sci Nutr. 2019;59(6):992-1007. doi:10.1080/10408398.2018.1537237
[3] Kenji Ina1,Takae Kataoka, and Takafumi Ando, The Use of Lentinan for Treating Gastric Cancer, Anti-Cancer Agents in Medicinal Chemistry, 2013, 13, 681-688 681
[4] Ohno N, Furukawa M, Miura NN, et al. Antitumor beta glucan from the cultured fruit body of Agaricus blazei . Biol Pharm Bull. 2001;24:820‐828
[5] Reynolds JA, Kastello MD, Harrington DG, et al. Glucan‐induced enhancement of host resistance to selected infectious diseases. Infect Immun. 1980;30:51‐57.
[6] Vetvicka V, Yvin J-C. Effects of marine β − 1, 3 glucan on immune reactions. Int Immunopharmacol. 2004;4(6):721–30.
[7] Pashine A, Valiante NM, Ulmer JB. Targeting the innate immune response with improved vaccine adjuvants. Nat Med. 2005;11:S63–8.
[8] Aleem E. β-Glucans and their applications in cancer therapy: focus on human studies; Anticancer Agents Med Chem. 2013 Jun; 13(5):709-19.
[9] Murphy EJ, Masterson C, Rezoagli E, O’Toole D, Major I, Stack GD, Lynch M, Laffey JG, Rowan NJ. β-Glucan extracts from the same edible shiitake mushroom Lentinus edodes produce differential in-vitro immunomodulatory and pulmonary cytoprotective effects – Implications for coronavirus disease (COVID-19) immunotherapies. Sci Total Environ. 2020 Aug 25;732:139330. doi: 10.1016/j.scitotenv.2020.139330. Epub 2020 May 11. PMID: 32413619; PMCID: PMC7211630.
[10] Newmaster SG, Grguric M, Shanmughanandhan D, Ramalingam S, Ragupathy S. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013;11:222.
[11] Tan L, Song X, Ren Y, Wang M, Guo C, Guo D, Gu Y, Li Y, Cao Z, Deng Y. Anti-inflammatory effects of cordycepin: A review. Phytother Res. 2020 Oct 8. doi: 10.1002/ptr.6890. Epub ahead of print. PMID: 33090621.
[12] Shahzad F, Anderson D, Najafzadeh M. The Antiviral, Anti-Inflammatory Effects of Natural Medicinal Herbs and Mushrooms and SARS-CoV-2 Infection. Nutrients. 2020 Aug 25;12(9):2573. doi: 10.3390/nu12092573. PMID: 32854262; PMCID: PMC7551890.
[13] Chikhale RV, Sinha SK, Patil RB, Prasad SK, Shakya A, Gurav N, Prasad R, Dhaswadikar SR, Wanjari M, Gurav SS. In-silico investigation of phytochemicals from Asparagus racemosus as plausible antiviral agent in COVID-19. J Biomol Struct Dyn. 2020 Jun 24:1-15. doi: 10.1080/07391102.2020.1784289. Epub ahead of print. PMID: 32579064; PMCID: PMC7335809.
[14] Harnett J, Oakes K, Carè J, Leach M, Brown D, Cramer H, Pinder TA, Steel A, Anheyer D. The effects of Sambucus nigra berry on acute respiratory viral infections: a rapid review of clinical studies. Adv Integr Med. 2020 Aug 22. doi: 10.1016/j.aimed.2020.08.001. Epub ahead of print. PMID: 32864330; PMCID: PMC7443157.
[15] Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, Qin Z, Peng X, Xiao H, Chen C, Liu X, Ning L, Wang B, Tang N, Li M, Xu F, Lin S, Yang J. Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study. J Am Coll Nutr. 2020 Oct 13:1-8. doi: 10.1080/07315724.2020.1826005. Epub ahead of print. PMID: 33048028.
[16] Zahra A, Sisu C, Silva E, De Aguiar Greca SC, Randeva HS, Chatha K, Kyrou I, Karteris E. Is There a Link between Bisphenol A (BPA), a Key Endocrine Disruptor, and the Risk for SARS-CoV-2 Infection and Severe COVID-19? J Clin Med. 2020 Oct 14;9(10):E3296. doi: 10.3390/jcm9103296. PMID: 33066495.
[17] https://www.medpagetoday.com/infectiousdisease/covid19/89055?xid=nl_covidupdate_2020-1012&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=DailyUpdate_101220&utm_term=NL_Gen_Int_Daily_News_Update, by Molly Walker, Associate Editor, MedPage Today October 9, 2020, CDC, How COVID-19 Spreads, https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html, retrieved 10/05/2020
[18] Barnkob MB, et al “Reduced prevalence of SARS-CoV-2 infection in ABO blood group O” Blood Adv 2020; DOI: 10.1182/bloodadvances.2020002657.
[19] Hoiland RL, et al “The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19” Blood Adv 2020; DOI: 10.1182/bloodadvances.2020002623.
[20] MedPage Today Editor-in-Chief and preprint co-author Marty Makary, MD, MPH, of Johns Hopkins University in Baltimore, speaks with Harlan Krumholz, MD, of Yale University, about the new data as well as the importance of sharing information like this in real-time via preprints during a pandemic. Interview by by Greg Laub, Director, Video, MedPage Today November 11, 2020, https://www.medpagetoday.com/infectiousdisease/covid19/89613?xid=nl_covidupdate_2020-11-12&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=DailyUpdate_111220&utm_term=NL_Gen_Int_Daily_News_Update

Donnie:
What vitamin supplements are you recommending to take to prevent of help with Covid19
Best,
Thank you for this rigorous article, Donnie Yance on the latest Covid-19 research, and forefront natural compounds, especially on mushrooms. Your early article at the onset of the pandemic, reporting on Elderberry, shed important light too. You’re a guide through this health challenge, giving many of us direction. Even basic facts on COVID-19 transmission have been misunderstood and miscommunicated. The kind of research that you put into your work is at a deep and comprehensive level. Much gratitude, from another health writer!
Hi Donnie, Will you be publishing your opinion on the new Covid-19 vaccine? I would really like to know your opinion on it’s safety? I have read all your responses to the flu vaccine in the past. I want to be vaccinated however I want to do more research. I don’t want to blindly get vaccinated without knowing the risks.