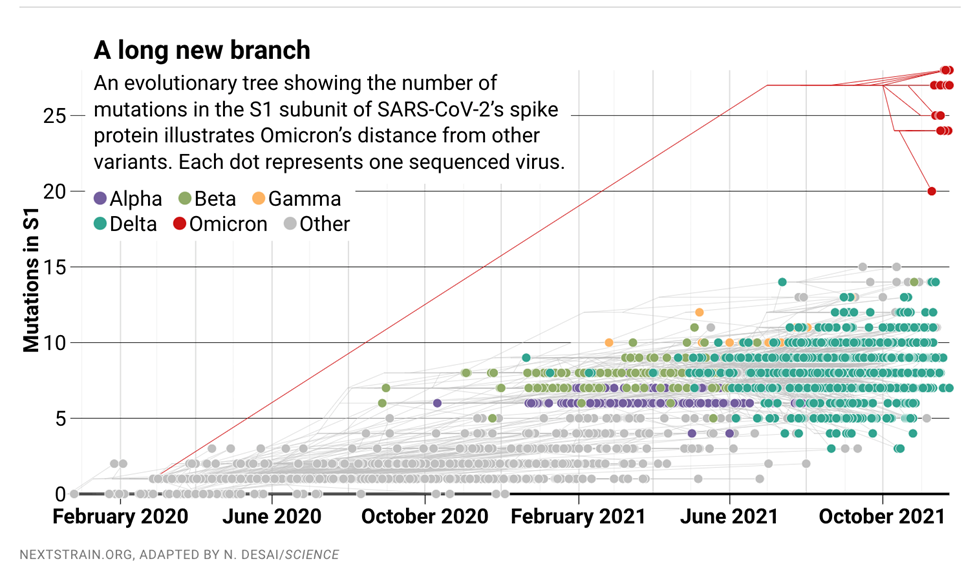
The Covid-19 pandemic has now been with us for close to two years and shows no signs of ever being completely extinguished. Many epidemiologists believe that the virus is here to stay, in the same way that the seasonal flu and common cold are also part of our lives. My belief is that continuing attempts to eradicate the virus through vaccination are not the best way to deal with an ever-changing target. Viruses continually mutate, and I believe our best approach to staying healthy is to bolster our innate immunity, and when necessary, to employ treatments with minimal side effects.
Recent Paper on Ivermectin Ignores Positive Studies
I believe that Ivermectin has been maligned and misunderstood as a prophylactic and treatment for Covid-19. On October 29th 2021, Medscape published a paper titled “Re-Analysis, Ivermectin Benefits Disappeared as Trial Quality Increased.”
This what the paper reports:
“For the re-analysis, Andrew Hill, PhD, of the University of Liverpool in England, and colleagues included 12 studies with 2,628 participants, and assessed them for bias. Overall, four studies had a low risk for bias, four studies had moderate risk, three studies were at high risk for bias, and one was potentially fraudulent.
Taken at face value, the overall meta-analysis found a 51% increase in survival with ivermectin (P=0.01), but excluding the potentially fraudulent trial, ivermectin’s benefit fell to 38% and was of borderline significance (P=0.05), they reported.
Taking out the studies with a high risk of bias led to a further drop — down to a nonsignificant 10% increase in survival (P=0.66), they noted. Further removing studies with a moderate risk of bias took the benefit down to 4% (P=0.9).”[1],[2]
The bottom line is that they took 4 studies out of a total of 12, where ivermectin had the least impact, and said they were the ones without bias. Yet they give no details as to how they came to this conclusion. They also added two studies on remdesivir, with a total of 6 studies that actually referred to ivermectin, and again ignored the now close to 100 studies on ivermectin and Covid.
My two recent papers, “Ivermectin and COVID-19 – Revision”[3] and “Ivermectin as a Prophylactic and Treatment for COVID-19”[4] highlight almost 40 studies, all of which show benefit. Why were none of these studies included?
Vaccines Have Little Effect against Delta Variant Transmission
Based on six new studies, people that are vaccinated appear to shed and spread Covid-19 Delta as much, or possibly even more, than the unvaccinated.
Study 1: This study found comparable viral loads among vaccinated vs. non-vaccinated healthcare workers (HCWs) infected by variant Delta B.1.1.7, suggesting suboptimal protection of SARS-CoV-2 vaccines against new variants as compared to wild-type SARS-CoV-2.
Among all 55 PCR-positive HCWs, 24 (44%) had received at least one dose of the BNT162b2 vaccine, and 21 were fully vaccinated (diagnosed with COVID- 19>2 weeks after the second dose). The three individuals that had one dose had received it 11, 20 and 22 days before the positive PCR result. In 23 of 24 positive HCW, PCR showed the SARS-CoV-2 B.1.1.7 variant, in one single subject the B.1.177 variant. Up till May 12, only 2 HCWs required hospitalization, both of which were not vaccinated. Vaccinated (with at least one dose) HCWs did not differ significantly compared to non-vaccinated HCWs in regard to age, gender and epidemiological exposures.[5]
Study 2: This recent study (D. W. Eyre et al. preprint at medRxiv; 2021)[6] looked directly at how well vaccines prevent the spread of the Delta variant of SARS-CoV-2. It showed that people infected with Delta are less likely to pass on the virus if they have already had a COVID-19 vaccine than if they haven’t. However the protective effect of the vaccine is small, and dwindles alarmingly over time.
In this study, researchers analyzed testing data from 139,164 close contacts of 95,716 people infected with SARS-CoV-2 between January and August 2021 in the United Kingdom, when the Alpha and Delta variants were competing for dominance. Although vaccines did offer some protection against infection and transmission, Delta dampened that effect. A vaccinated person who had a ‘breakthrough’ Delta infection was almost twice as likely to pass on the virus as was someone who was infected with Alpha. And the vaccines effect on Delta transmission waned to almost negligible levels over time.
The results “possibly explain why we’ve seen so much onward transmission of Delta despite widespread vaccination,” says co-author David Eyre, an epidemiologist at the University of Oxford, UK.[7]
Study 3: Data released August 6th, 2021, by the CDC showed that vaccinated people infected with the Delta variant can carry detectable viral loads similar to those of people who are unvaccinated. The study stated, “Among five COVID-19 patients who were hospitalized, four were fully vaccinated; no deaths were reported. Real-time reverse transcription-polymerase chain reaction (RT-PCR) cycle threshold (Ct) values in specimens from 127 vaccinated persons with breakthrough cases were similar to those from 84 persons who were unvaccinated, not fully vaccinated, or whose vaccination status was unknown (median = 22.77 and 21.54, respectively).”[8]
Study 4: Ireland’s Waterford city district has emerged as the place with the highest rate of Covid-19 infection, despite the fact that it has the highest rate of vaccination in the Republic. The city’s south electoral area has a 14-day incidence rate of 1,486 cases per 100,000 of the population, three times the national average which stands at 493 infections per 100,000 people. Waterford has 99.7 per cent of its adult population fully vaccinated.[9]
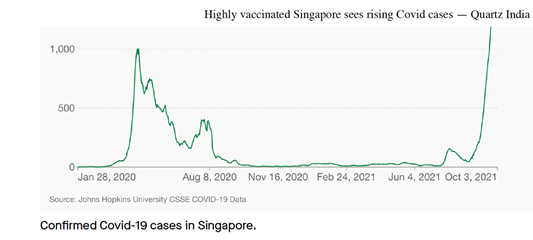
Study 5: Singapore, with 82% of its population of 5.7 million fully vaccinated, was once believed to have passed the threshold for herd immunity. But it’s now seeing a surge in Covid-19 cases. In the month of October, Singapore reported record high cases since late September, with more than 2,900 new infections on Oct. 1.
Prior to this wave, the highest single-day total was 1,426 reported in April 2020.[10]
Study 6: A new study, which appears in The Lancet Infectious Diseases Trusted Source,[11] has found that vaccination alone is not enough to stop the household transmission of the Delta variant.
What we have learned so far is thatthe peak viral load of the Delta virus does not differ between fully vaccinated and nonvaccinated individuals. Also, the elimination of the Delta strain of the virus takes place more quickly in vaccinated individuals.
Natural Immunity and Covid-19 Update
While a much-publicized CDC report concluded that mRNA vaccination provides stronger protection against COVID-19 hospitalization than prior infection, there were several study limitations, including that it was not a randomized controlled trial and that the follow-up period was short. The findings also don’t negate the robust protection from prior infection which many studies have now confirmed. In fact, in a recent CDC science report[12] that reviews the totality of evidence, agency staff found that infection-induced immunity is durable for at least 6 months.
“Researchers at the Cleveland Clinic Health System conducted a study of 52,238 employees with and without a history of COVID-19, with or without vaccination. They found that those who recovered from COVID-19 and were vaccinated had equally low rates of repeat infection when compared with those who recovered and were unvaccinated. The investigators concluded that those previously infected were unlikely to benefit from COVID-19 vaccination.[13] In another study looking at the duration of immunity among the COVID-19-recovered, researchers found that the immune response against SARS-CoV-2 was persistent and relatively stable for at least a year.”[14]
Multiple studies also show that people who have recovered from COVID-19 are at least equally protected compared to fully vaccinated COVID-naive people.[15] This recent meta-analysis included nine clinical studies, including three randomized controlled studies, four retrospective observational cohorts, one prospective observational cohort, and a case-control study.
A new study, published in the November 2021 issue of the prestigious Lancet Journal, highlights protective immunity after recovery from SARS-CoV-2 infection. According to the review, an overwhelming amount of research confirms those who have natural immunity are well protected. Several studies have found that people who recovered from COVID-19 and tested seropositive for anti-SARS-CoV-2 antibodies have low rates of SARS-CoV-2 reinfection. This study puts to rest the questions surrounding the strength and duration of such protection compared with that from vaccination.
Within this review paper, studies published in PubMed to September 28, 2021 were analyzed, including well-conducted biological studies showing protective immunity after infection. Furthermore, multiple epidemiological and clinical studies, including studies during the recent period of predominantly delta (B.1.617.2) variant transmission, found that the risk of repeat SARS-CoV-2 infection decreased by 80.5–100% among those who previously had COVID-19.
The reported studies were large and conducted throughout the world. Another laboratory-based study that analyzed the test results of 9,119 people with previous COVID-19 from December 1, 2019 to November 13, 2020 found that only 0.7% became reinfected.[16]
Here is a breakdown of the research studies they reviewed:
Biological studies
- Dan et al (2021): About 95% of participants tested retained immune memory at about 6 months after having COVID-19; more than 90% of participants had CD4+ T-cell memory at 1 month and 6–8 months after having COVID-19.[17]
- Wang et al (2021): Participants with a previous SARS-CoV-2 infection with an ancestral variant produce antibodies that cross-neutralize emerging variants of concern with high potency.[18]
Epidemiological studies
- Hansen et al (2021): In a population-level observational study, people who previously had COVID-19 were around 80·5% protected against reinfection.[19]
- Pilz et al (2021): In a retrospective observational study using national Austrian SARS-CoV-2 infection data, people who previously had COVID-19 were around 91% protected against reinfection.[20]
- Sheehan et al (2021): In a retrospective cohort study in the USA, people who previously had COVID-19 were 81·8% protected against reinfection.[21]
- Shrestha et al (2021): in a retrospective cohort study in the USA, people who previously had COVID-19 were 100% protected against reinfection.[22]
- Gazit et al (2021): In a retrospective observational study in Israel, SARS-CoV-2-naive vaccinees had a 13.06-times increased risk for breakthrough infection with the delta (B.1.617.2) variant compared with those who previously had COVID-19; evidence of waning natural immunity was also shown.[23]
- Kojima et al (2021): in a retrospective observational cohort of laboratory staff routinely screened for SARS-CoV-2, people who previously had COVID-19 were 100% protected against reinfection.[24]
Clinical studies:
- Hall et al (2021): in a large, multicenter, prospective cohort study, having had COVID-19 previously was associated with an 84% decreased risk of infection.[25]
- Letizia et al (2021): in a prospective cohort of US Marines, seropositive young adults were 82% protected against reinfection.[26]
Potential Treatment of COVID-19 with Traditional Chinese (Herbal) Medicine
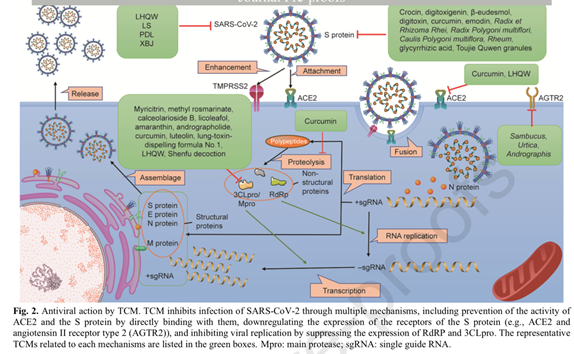
Traditional Chinese medicine (TCM) has shown success in treating viral infectious pneumonia. It has also exhibited therapeutic effects against infectious diseases, such as SARS and COVID-19. On February 7, 2020, the National Health Commission of the People’s Republic of China and the National Administration of Traditional Chinese Medicine recommended the Qingfei Paidu decoction, the Huashi Baidu formula, the Xuanfei Baidu decoction, the Jinhua Qinggan granule, the Lianhua Qingwen capsule/granule, and Xuebijing.
The experimental antivirus effects are mainly characterized by the direct inhibition of virus replication. Regarding the immune system destruction, inflammatory cytokine storm, and lung damage caused by COVID-19, some classic TCM formulas and proprietary Chinese medicines may regulate the immune system, reduce inflammatory responses, and suppress lung fibrosis and injury. Xuebijing, for example, has been found to have clinical efficacy in the treatment of COVID-19 for the treatment of flu-like symptoms, asthma, inflammation, tonsillitis, and sore throat.
Based on clinical results, TCM formulas have been applied to treat COVID-19, and their effects have been remarkable. Experimental studies have focused on the potential antiviral effects of classical formulas. For example, the Huashi Baidu formula has been recommended by the National Health Commission of the People’s Republic of China for the treatment of COVID-19 patients with mild and severe symptoms. Cai et al. identified 223 active ingredients in Huashi Baidu formula that potentially interact with 84 COVID-19-related target genes, such as ACE2, estrogen receptor 1, adrenergic receptor α1, and histone deacetylase 1.[27]
One of the many advantages of TCM and herbal medicine lies not only in its regulation of immunity, but also in its holistic regulation of metabolism and the intestinal environment and broad protective effects as well on organ systems.[28]
Indonesia First to Greenlight Novavax COVID-19 Vaccine
JAKARTA, Indonesia (AP) — Biotechnology company Novavax said Monday that Indonesia has given the world’s first emergency use authorization for its COVID-19 vaccine, which uses a different technology than current shots. The vaccine is easier to store and transport than some other shots, which could allow it to play an important role in boosting supplies in poorer countries around the world.
Novavax said it has already filed for authorization of the vaccine in the United Kingdom, European Union, Canada, Australia, India, and the Philippines.[29]
Also keep in mind, some people are allergic to polyethylene glycol (PEG), an ingredient in the mRNA (Pfizer and Moderna) vaccines. There’s no polyethylene glycol (PEG) in Novavax.
How the Novavax COVID-19 Vaccine Works
Unlike the mRNA and vector vaccines, this is a protein adjuvant (an adjuvant is an ingredient used to strengthen the immune response and in this case it a plant saponin extract, called Matrix M, from the Soapbark tree).
While other vaccines trick the body’s cells into creating parts of the virus that can trigger the immune system, the Novavax vaccine takes a different approach. It contains the spike protein, made from a moth and not the RNA messenger.
Unlike mRNA vaccines that command your own cells to manufacture the antigens that trigger an immune response, the Novavax vaccine contains the antigens themselves. The lab-grown nanoparticle spike protein mimics the natural spike protein on the surface of the coronavirus cannot cause disease.
How did they get the spike protein?
The Novavax method uses moth cells to make spike proteins:
- Researchers select the desired genes that create certain SARS-CoV-2 antigens (spike protein).
- Researchers put the genes into a baculovirus, an insect virus.
- The baculovirus infects moth cells and replicates inside them.
- These moth cells create lots of spike proteins.
- Researchers extract and purify the spike proteins.
The Novavax vaccine has no genetic material, only proteins.
When the vaccine is injected, the Matrix-M Soapbark extract stimulates the immune system to produce antibodies and T-cell immune responses.
This tried-and-true method of making a custom copy of a virus spike protein has been used to develop vaccines against HPV, hepatitis B and influenza.[30]
So, there you have it.
References
[1] https://www.medpagetoday.com/special-reports/exclusives/95333?xid=nl_medpageexclusive_2021-11-01&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=MPTExclusives_110121&utm_term=NL_Gen_Int_Medpage_Exclusives_Active
[2] Hill A, et al “Ivermectin for COVID-19: addressing potential bias and medical fraud” Research Square 2021; DOI: 10.21203/rs.3.rs-1003006/v1.
[3] https://www.donnieyance.com/ivermectin-and-covid-19-revision/
[4] https://www.donnieyance.com/ivermectin-as-a-prophylactic-and-treatment-for-covid-19/
[5] Petros Ioannoua , Stamatis Karakonstantisa , Eirini Astrinakib, Stamatina Saplamidoub, Efsevia Vitsaxakib, Georgios Hamilosc, George Sourvinosd and Diamantis P. Kofteridisa, Transmission of SARS-CoV-2 variant B.1.1.7 among vaccinated health care workers, INFECTIOUS DISEASES, 2021; VOL. 0, NO. 0, 1–4, https://doi.org/10.1080/23744235.2021.1945139
[6] David W Eyre, Donald Taylor, Mark Purver, David Chapman, Tom Fowler, Koen B Pouwels, A Sarah Walker, Tim EA Peto. The impact of SARS-CoV-2 vaccination on Alpha & Delta variant transmission, doi: https://doi.org/10.1101/2021.09.28.21264260
[7] Nature, https://www.nature.com/articles/d41586-021-02759-1?WT.ec_id=NATURE-20211014&utm_source=nature_etoc&utm_medium=email&utm_campaign=20211014&sap-outbound-id=C45F96E14F855E90076BC7A0A2589E9DC8299B74, 10/13/2021
[8] Brown CM, Vostok J, Johnson H, Burns M, Gharpure R, Sami S, Sabo RT, Hall N, Foreman A, Schubert PL, Gallagher GR, Fink T, Madoff LC, Gabriel SB, MacInnis B, Park DJ, Siddle KJ, Harik V, Arvidson D, Brock-Fisher T, Dunn M, Kearns A, Laney AS. Outbreak of SARS-CoV-2 Infections, Including COVID-19 Vaccine Breakthrough Infections, Associated with Large Public Gatherings – Barnstable County, Massachusetts, July 2021. MMWR Morb Mortal Wkly Rep. 2021 Aug 6;70(31):1059-1062. doi: 10.15585/mmwr.mm7031e2.
[9] https://www.irishtimes.com/news/health/waterford-city-district-has-state-s-highest-rate-of-covid-19-infections-1.4707344, The Irish Times, October 21, 2021
[10] https://qz.com/india/2068834/highly-vaccinated-singapore-sees-rising-covid-cases/, Kapur, Manavi, Oct. 5th, 2021
[11] Anika Singanayagam, Seran Hakki, Jake Dunning, Kieran J Madon, Michael A Crone, Aleksandra Koycheva, Nieves Derqui-Fernandez, Jack L Barnett, Michael G Whitfield, Robert Varro, Andre Charlett,Rhia Kundu, Joe Fenn, Jessica Cutajar,Valerie Quinn, Emily Conibear, Wendy Barclay, Paul S Freemont, Graham P Taylor, Shazaad Ahmad, Maria Zambon, Neil M Ferguson, Ajit Lalvani, on behalf of the ATACCC Study Investigators, Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study; The Lancet Infectious Diseases Trusted Source, Published on line: October 29, 2021 DOI:https://doi.org/10.1016/S1473-3099(21)00648-4
[12] Bozio CH, et al “Laboratory-confirmed COVID-19 among adults hospitalized with COVID-19–like illness with infection-induced or mRNA vaccine-induced SARS-CoV-2 immunity — nine States, January–September 2021” MMWR 2021; DOI: 10.15585/mmwr.mm7044e1.
[13] Nabin K. Shrestha, Patrick C. Burke, Amy S. Nowacki, Paul Terpeluk, Steven M. Gordon Necessity of COVID-19 vaccination in previously infected individuals, https://doi.org/10.1101/2021.06.01.21258176
[14] https://www.medpagetoday.com/opinion/second-opinions/95399, Medscape, Jeffrey D. Klausner, MD, MPH, and Noah Kojima, MD November 2, 2021, COVID Vaccine Mandates and the Question of Medical Necessity,
[15] Mahesh B. Shenai, Ralph Rahme, Hooman Noorchashm Equivalency of Protection from Natural Immunity in COVID-19 Recovered Versus Fully Vaccinated Persons: A Systematic Review and Pooled Analysis doi: https://doi.org/10.1101/2021.09.12.21263461
[16] Noah Kojima, Jeffrey D Klausner, Protective immunity after recovery from SARS-CoV-2 infection, The Lancet Infectious Diseases, 2021, ISSN 1473-3099, https://doi.org/10.1016/S1473-3099(21)00676-9. (https://www.sciencedirect.com/science/article/pii/S1473309921006769)
[17] M Dan, J Mateus, Y Kato, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection Science, 371 (2021), Article eabf4063
[18] L Wang, T Zhou, Y Zhang, et al. Ultrapotent antibodies against diverse and highly transmissible SARS-CoV-2 variants, Science, 373 (2021), Article eabh1766
[19] CH Hansen, D Michlmayr, SM Gubbels, K Mølbak, S Ethelberg, Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study, Lancet, 397 (2021), pp. 1204-1212
[20] S Pilz, A Chakeri, JP Ioannidis, et al. SARS-CoV-2 re-infection risk in Austria. Eur J Clin Invest, 51 (2021), Article e13520
[21] MM Sheehan, AJ Reddy, MB Rothberg, Reinfection rates among patients who previously tested positive for COVID-19: a retrospective cohort study, Clin Infect Dis (2021), published online March 15. https://doi.org/10.1093/cid/ciab234
[22] N Kojima, A Roshani, M Brobeck, A Baca, JD Klausner, Incidence of severe acute respiratory syndrome coronavirus-2 infection among previously infected or vaccinated employees medRxiv (2021), published online July 8. https://doi.org/10.1101/2021.07.03.2125997
[23] S Gazit, R Shlezinger, G Perez, et al. Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections, medRxiv (2021) published online Aug 25. https://doi.org/10.1101/2021.08.24.21262415
[24] N Kojima, A Roshani, M Brobeck, A Baca, JD Klausner, Incidence of severe acute respiratory syndrome coronavirus-2 infection among previously infected or vaccinated employees medRxiv (2021), published online July 8. https://doi.org/10.1101/2021.07.03.21259976
[25] VJ Hall, S Foulkes, A Charlett, et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN) Lancet, 397 (2021), pp. 1459-1469
[26] AG Letizia, Y Ge, S Vangeti, et al. SARS-CoV-2 seropositivity and subsequent infection risk in healthy young adults: a prospective cohort study, Lancet Respir Med, 9 (2021), pp. 712-720
[27] Cai Y, Zeng M, Chen YZ. The pharmacological mechanism of Huashi Baidu formula for the treatment of COVID-19 by combined network pharmacology and molecular docking. Ann Palliat Med 2021;10(4):3864–95.
[28] L. Li, Y. Wu, J. Wang, H. Yan, J. Lu, Y. Wan, B. Zhang, J. Zhang, J. Yang, X. Wang, M. Zhang, Y. Li, L. Miao, H. Zhang, Potential treatment of COVID-19 with traditional chinese medicine: What herbs can help win the battle with SARS-CoV-2?, Engineering (2021), doi: https://doi.org/10.1016/j.eng. 2021.08.020
[29] https://omaha.com/news/world/indonesia-first-to-green-light-novavax-covid-19-vaccine/article_14481bb0-0cb1-545b-b394-9db4dcda861c.html, retrieved 11/13/2021
[30] https://www.nebraskamed.com/COVID/moths-and-tree-bark-how-the-novavax-vaccine-works retrieved 11/13/2021