Here is my counter-review of the recent headline news article that might make you wary of taking vitamins, titled “Vitamin D Supplements May Be a Double-Edged Sword.” This article was written by F. Perry Wilson, MD, MSCE, and published on March 14, 2024, in MDedge Family Medicine (https://www.mdedge.com/familymedicine/article/268256/womens-health/vitamin-d-supplements-may-be-double-edged-sword?ecd=WNL_EVE_240316_mdedge).
This was a summary review of a peer-reviewed paper titled “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women: Postintervention Follow-up of a Randomized Clinical Trial,” published in the Annals of Internal Medicine Journal.[1]
The conclusion of this study reads, “Calcium and vitamin D supplements seemed to reduce cancer mortality and increase cardiovascular disease (CVD) mortality after more than 20 years of follow-up among postmenopausal women, with no effect on all-cause mortality.” NOTE that the lead word is calcium, not Vitamin D, which Dr. Wilson chose to emphasize.
Dr. Wilson concluded from the study, “I can tell you that for your “average woman,” vitamin D supplementation likely has no effect on mortality. It might modestly reduce the risk for certain cancers while increasing the risk for heart disease (probably through coronary calcification). So, there might be some room for personalization here. Perhaps women with a strong family history of cancer or other risk factors would do better with supplements, and those with a high risk for heart disease would do worse.”
Problems with this Study and Calcium Supplementation
What Dr. Wilson’s article omits is that this isn’t a vitamin D study at all; it’s a calcium study where patients took 1000 mg of calcium carbonate (a poor form of calcium) along with only 400 IUs of vitamin D. This misrepresentation and bias against supplements are frustrating and repetitive.
Calcium carbonate supplementation, especially at 1000 mg daily, isn’t good for heart health or any health condition. It can increase the risk of vascular calcifications.
I’ve written extensively on vitamin K’s role and its partnership with vitamin D. Read my blog, “Vitamin K: An Essential Nutrient For Cardiovascular Health.”
For a deeper understanding of supplements and their forms, check out my blog, “Do you Know What’s in Your Vitamin Supplements?”
For info on vitamin D and COVID-19, read my paper, “COVID-19 Updates on Natural Immunity and Vitamin D, plus Facts and Reflections on Science, Truth, Knowledge, and Wisdom.”
This study and many others suggest that high calcium supplements, particularly calcium carbonate, increase vascular calcifications, a major cause of CVD. Calcium supplements should only be taken if there’s a deficiency, not even for bone health. Results from randomized controlled trials show no reduction in hip fracture risk with calcium supplementation, and an increased risk is possible.[2],[3]
In an aging society, one challenge in percutaneous coronary interventions is calcified coronary lesions.[4] Vascular calcifications are the most common type of soft tissue calcification, where calcium and phosphate accumulate in blood vessels and cardiac valves. Vascular calcification is the ectopic deposition of mineral matrix in the vessel wall.[5],[6] It’s a common consequence of aging, atherosclerosis, diabetes, and chronic kidney disease and is a strong predictor of increased cardiovascular morbidity and mortality.[7],[8],[9],[10]
Vascular calcification is a significant risk factor for cardiovascular morbidity and mortality in patients with end-stage renal disease, diabetes, and atherosclerosis. Currently, there’s no pharmaceutical strategy to prevent this pathological process[11], and statin therapy may not help or may even contribute to it.[12],[13]
This study didn’t check before and after vitamin D levels (both forms 25 OH and the active form 125 di OH), which likely didn’t change much due to the low dosage. They also didn’t check calcium levels, urine excretion of calcium, urine pH, parathyroid hormone, and vitamin K as serum undercarboxylated osteocalcin (ucOC) levels. There’s a relationship between elevated serum ucOC levels and vitamin K deficiency.[14],[15]
Vitamin K2 activates osteocalcin, produced by osteoblasts, which is needed to bind calcium into the matrix of your bone. Osteocalcin also helps prevent calcium from depositing into your arteries. Vitamin K2 activates matrix GLA protein (MGP) to bind excess calcium and promote arterial flow and flexibility.[16]
Think of vitamin D as the gatekeeper, controlling who gets in, and vitamin K as the (calcium) traffic cop, directing traffic. Lots of traffic, but no traffic cop means clogging, crowding, and chaos! Without D and K, calcium might build up in your coronary arteries rather than your bones.[17]
Osteocalcin is a small protein found in bones, also called bone Gla-protein. It’s the most common non-collagen protein in bones and is a hormone made in the bones. Osteocalcin helps hold calcium and is important for building and healing bones. Osteoblasts make osteocalcin and put it into the bone structure. Osteocalcin goes into the bloodstream when bones break down and is a sign of bone activity, not just growth.[18] Vitamin K plays an important role in osteoporosis and serum osteocalcin levels.[19] Osteocalcin also has a hormonal role, acting in a feed-forward loop to increase β-cell proliferation, insulin production, and secretion, increasing neurotransmitter production, and stimulating testosterone production in the testes.[20] There’s a relationship between low osteocalcin levels and metabolic syndrome/insulin resistance.[21],[22],[23]
The Truth Regarding Vitamin D and Heath
Vitamin D is one of the foremost nutrients that plays a crucial role in various biochemical pathways and is an important key factor in several diseases.
An overwhelming amount of evidence supports supplementing vitamin D to correct vitamin D deficiency, which in turn is associated with reduced all-cause mortality and a reduction in most chronic and even acute diseases. A 2019 systemic review on vitamin D supplementation and all-cause mortality was conducted. Fifty-two trials with a total of 75, 454 participants were identified. Vitamin D supplementation reduced the risk of cancer death by 16%. In subgroup analyses, all-cause mortality was significantly lower in trials with vitamin D3 supplementation than in trials with vitamin D2 supplementation.[24]
All-cause mortality is independently and inversely associated with serum 25 OH vitamin D levels at less than 50 nmol/liter. Low 25-OH vitamin D is associated with increased mortality in female nursing home residents 25-OH vitamin D levels were inversely associated with all-cause and CVD mortality among adults with hypertension.[25],[26] The risk of all-cause mortality is inversely related to serum 25 OH vitamin D levels.[27]
A regular intake of vitamin D can reduce the risk of early death substantially in people with cardiovascular disease, a new study shows. The study concludes that people who have suffered from cardiovascular disease and have a normal intake of vitamin D reduce their risk of mortality as a consequence of the disease by 30 percent.[28]
Low levels of vitamin D 25-OH (vitamin D deficiency) are associated with increased mortality in patients with chronic heart failure due to left ventricular systolic dysfunction.[29]
Concentrations of 25-OH vitamin D are inversely associated with all-cause and CVD mortality among adults with hypertension in the US.[30]
Many studies have found a striking correlation between low serum 25-OH D levels and several different cardiovascular diseases.[31]
Vitamin D status modifies the association between statin use and musculoskeletal pain. Among adults ≥ 40 years old with 25-OH vitamin D <15 ng/mL, statin users had nearly two times greater odds of reporting musculoskeletal pain compared to non-statin users.[32]
Epidemiological studies have shown that 25-OH vitamin D deficiency is closely associated with common chronic diseases such as bone metabolic disorders, tumors, cardiovascular diseases, and diabetes. 25OHD deficiency is also a risk factor for neuropsychiatric disorders and autoimmune diseases. 25-OH vitamin D deficiency is highly prevalent in the world.[33]
Low levels of vitamin D correlate with increased risk for depression,[34],[35] immune dysfunction,[36],[37] diabetes,[38] poor cognition,[39] osteoporosis,[40],[41] and cancer incidence and progression,[42],[43] and reduced Quality-of-Life.[44],[45]
Vitamin D is an essential nutrient for preventing malignancies and a complementary treatment for cancer through direct and indirect biochemical pathways.[46]
A meta-analysis of randomized controlled trials of vitamin D supplementation and total cancer outcomes found that daily dosing, but not infrequent large-bolus dosing, Vitamin D supplementation reduced total cancer mortality.[47]
In a previous review of 10 meta-analysis randomized controlled trials, vitamin D supplementation significantly reduced total cancer mortality.[48]
Numerous studies have found a connection between low serum 25-OH vitamin D levels and an increased risk of incident colon, prostate, and breast cancer, as well as higher mortality from these cancers. Specifically, levels below 20 ng/ml are associated with a 30 to 50% increased risk.[49],[50] One compelling reason to maintain sufficient vitamin D levels is a report showing that postmenopausal women who increased their vitamin D intake by 1100 IU of vitamin D3 reduced their relative risk of cancer by 60 to 77%.[51]
A recent study examined the associations of vitamin D deficiency, insufficiency, and vitamin D supplementation use with mortality from any cancer and 18 specific cancers in 411,436 United Kingdom Biobank participants aged 40-69 years. The study found that Vitamin D deficiency and insufficiency were associated with increased mortality from multiple common cancers.[52]
Vitamin D plays an important role in prostate conditions and prostate cancer. Many studies show it plays a role in many aspects of male reproductive health, including male hypogonadism and prostate cancer prevention and potentially for treatment.[53],[54],[55],[56],[57],[58],[59],[60],[61]
Vitamin D supplementation has been shown to improve overactive bladder in men.[62]
Vitamin D and Breast Cancer
Increasing vitamin D levels may help curb the development and progression of breast cancer.[63]
Vitamin D levels 25-OH were tested in blood samples from 290 Black/African American women, 125 non-Black Hispanic/Latina women who developed breast cancer, 1,084 Black/African American women, and 461 Hispanic/Latina women who did not develop breast cancer.
Over an average follow-up of 9.2 years, women with circulating 25(OH)D levels above the clinical cut point for deficiency (20.0 ng/mL) had a 21% lower breast cancer rate than women with concentrations below this cut point.[64]
There is a growing body of evidence that adequate vitamin D stores may prevent breast cancer development. Whereas circulating 25-OH vitamin D levels of >32 ng/mL are associated with normal bone mineral metabolism, data suggests that the optimal level for breast cancer prevention is >/=40 ng/mL.[65]
A total of 30 prospective studies (nested case-control or cohort) were included for breast cancer incidence (n=24 studies; 31 867 cases) or mortality (n=6 studies; 870 deaths) among 6092 breast cancer patients. The pooled RRs of breast cancer incidence for the highest vs the lowest vitamin D intake and blood 25- OH D levels were 0.95 (95% CI: 0.88–1.01) and 0.92 (95% CI: 0.83–1.02), respectively. Among breast cancer patients, high blood 25-OH D levels were significantly associated with lower breast cancer mortality (pooled RR=0.58, 95% CI: 0.40–0.85) and overall mortality (pooled RR=0.61, 95% CI: 0.48–0.79).[66]
A study was conducted to evaluate serum levels of vitamin D and other nutrients in Korean patients with benign breast disease or breast cancer. Severe vitamin D deficiency was more prevalent in breast cancer patients than in healthy controls. Vitamin D levels were significantly lower in breast cancer patients with estrogen receptor-negative or triple-negative subtypes than in those with other subtypes.[67]
In a mice study, vitamin D deficiency promotes the growth of human breast cancer cells in the bones of nude mice. These effects are partly mediated through secondary changes in the bone microenvironment, along with the direct effects of vitamin D on tumor growth.[68]
Vitamin D supplementation improves outcomes in women with HER2-positive breast cancer. In multivariate regression models, patients who took vitamin D supplements reduced their risk of losing disease-free status by 64%. Median disease-free survival was 32.6 months among the 134 patients undergoing adjuvant chemotherapy taking any form of vitamin D supplementation versus a median of 25.5 months for the women not taking supplements.[69]
Vitamin D insufficiency increases the risk of chemotherapy-related peripheral neuropathy in breast cancer patients.[70]
Vitamin D has even been shown to suppress (CD133+/CD44 +) cancer stem cell stemness by inhibiting NF-κB signaling and reducing NLRP3 expression in triple-negative breast cancer.[71]
Vitamin D and Colorectal Cancer
In observational studies, higher plasma 25-OH vitamin D levels have been associated with improved survival in metastatic colorectal cancer.[72]
In a phase 2 randomized clinical trial that included 139 patients with advanced or metastatic colorectal cancer, treatment with chemotherapy plus high-dose vitamin D3 supplementation vs chemotherapy plus standard-dose vitamin D3 resulted in a median progression-free survival of 13 months vs 11 months, respectively, that was not statistically significant, but a multivariable hazard ratio of 0.64 for progression-free survival or death that was statistically significant.[73]
New findings indicate that an increased intake of vitamin D may help to prevent the development of early-onset colorectal cancer in individuals under the age of 50.[74]
For patients with early-stage adenocarcinoma and low vitamin D levels, oral vitamin D supplementation significantly increased recurrence-free survival and overall survival.[75]
Vitamin D and Melanoma
Vitamin D supplementation increases objective response rate and prolongs progression-free time in patients with advanced melanoma undergoing anti-PD-1 therapy.
The potential mechanism of vitamin D’s influence on the effectiveness of therapy is most likely related to the amount and activity of tumor-infiltrating lymphocytes. Data shows the effect of vitamin D on cells regulating the activity of CD8 lymphocytes.
Vitamin D and Respiratory Infections and Immune Response
Vitamin D supplementation improves viral respiratory tract infections across cohorts, particularly in those with vitamin D deficiency, according to a systematic review of 39 randomized controlled trials.[77]
Patients with vitamin D deficiency (less than 20 ng/mL) were 14 times more likely to have a severe or critical case of COVID-19 than those with more than 40 ng/mL.[78]Black individuals who had levels of 30 to 40 ng/ml 25OHD had a 2.64 times higher risk of testing positive for COVID-19 than people with levels of 40 ng/ml or greater.[79] Older adults with vitamin D deficiency and COVID-19 demonstrate worse morbidity outcomes.[80],[81],[82],[83],[84] Vitamin D status may be a useful prognosticator.
In a study, researchers from the Azrieli Faculty of Medicine of Bar-Ilan University in Safed, Israel, and the Galilee Medical Center in Nahariya, Israel, showed a correlation between vitamin D deficiency and COVID-19 severity and mortality.[85]
Vitamin D supplementation has a preventive effect against COVID-19[86] and treatment with vitamin for COVID-19 reduced disease severity, hospitalization, hospital stay and mortality.[87], [88]
Vitamin D has immunomodulating properties and may enhance the body’s defense system against invading pathogenic organisms. In a group of 88 patients hospitalized for severe infection from the SARS-CoV-2 virus and a control group matched for age and sex, the levels of 25-OH vitamin D were analyzed. Levels of 25-OH vitamin D were 17.36 ± 8.80 ng/mL (mean ± SD) compared with 24.34 ± 10.34 ng/mL in patients with severe SARS-CoV-2 infection and the control group, respectively, p < 0.001 (Student’s t-test). 25(OH)D3 levels were significantly related to outcomes, i.e., survival as opposed to non-survival, as more patients with 25(OH)D3 deficiency (0-10 ng/mL) and insufficiency (10-20 ng/mL) had a fatal outcome as compared with those with vitamin D sufficiency (p < 0.001, chi-square test, p < 0.001, Fisher’s exact test).
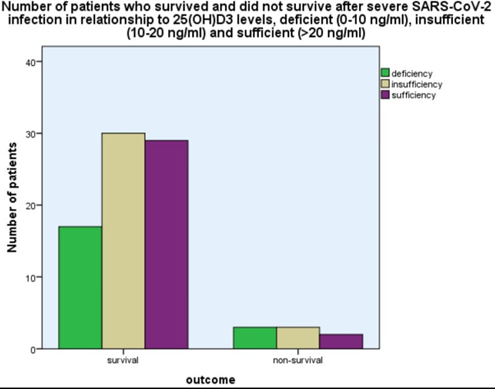
Levels of 25-OH vitamin D were inversely related to CRP, ferritin, d-dimer, and fibrinogen levels. Vitamin D deficiency observed in severe SARS-CoV-2 infection was related to disease outcomes.[89]
Low vitamin D levels can cause immune dysfunction, including a lack of antibody production and an increased risk of inflammation. With regard to respiratory function, low levels of vitamin D are associated with numerous pulmonary diseases, including acute lung injury and acute respiratory distress syndrome. Vitamin D and its receptors have been shown to protect epithelial barriers in various tissues and offer protection against acute respiratory distress syndrome and fibrosis.[90]Vitamin D also appears to calm inflammation. In one study, vitamin D-deficient mice were provided with vitamin D3, which suppressed signs of lung inflammation.[91]
Vitamin D can lower the risk of infections by inducing cathelicidins and defensins that reduce viral replication rates and diminish concentrations of pro-inflammatory cytokines. These inflammatory compounds injure the lining of the lungs and increase the risk of pneumonia. Vitamin D enhances protection by increasing concentrations of anti-inflammatory cytokines.[92]
As an immune system modulator, vitamin D strongly influences immune function and is well known for its ability to enhance immune response when at optimal serum and tissue levels.
Vitamin D and Other Conditions and Diseases
A recent clinical trial found that vitamin D supplementation improved total, physical, and mood symptoms in vitamin D insufficient women with PMS.[93]
Based upon several lines of evidence that documented chronically inadequate vitamin D intake in the US, particularly in the northern states and particularly in the elderly, is a significant factor in the pathogenesis of Parkinson’s Disease.[94],[95]
A study has linked vitamin D blood levels with multiple sclerosis (MS) progression. MS is a chronic (long-term), progressive, degenerative disorder that affects nerve fibers in the brain and spinal cord. The researchers found that participants with higher vitamin D blood levels had a slower rate of MS progression, noting that increases in vitamin D levels by 50 nmol/L were linked to a 57 percent reduced risk of developing new active brain lesions and a 57 percent lower risk of relapse.[96]
The insufficiency or deficiency of vitamin D is common in various kinds of chronic liver diseases including viral hepatitis B and C. Serum 25-OH vitamin D and vitamin D receptors are possibly interrelated with disease incidence, treatment and prognosis.[97]
A meta-analysis was published on the efficacy of oral supplemental vitamin D in preventing nonvertebral and hip fractures among older individuals (> or =65 years). We included 12 double-blind randomized controlled trials for nonvertebral fractures. Nonvertebral fracture prevention with vitamin D is dose-dependent, and a higher dose should reduce fractures by at least 20% for individuals aged 65 years or older.[98]
An analysis of the literature shows that vitamin D plays a significant role in maintaining healthy periodontal and jawbone tissues, alleviating inflammation processes, stimulating post-operative healing of periodontal tissues, and the recovery of clinical parameters.[99]Vitamin D deficiency correction through supplementation can contribute to a successful treatment of periodontitis. Vitamin D-deficient patients seem more prone to failure. Vitamin D can also be linked with some oral pathology entities, such as certain oral cancers and events of jaw osteonecrosis.[100]
Why aren’t any of the very robust studies making headline news? Instead, this bogus study falsely accuses vitamin D supplements as a potential risk factor for heart disease.
What is an Optimal Range for Vitamin D?
The US Institute of Medicine (IOM) recommendations for vitamin D, based on a review of the evidence, concluded that:
- serum 25(OH)D <30 ng/mL is deficient
- serum 25(OH)D of 30–40 ng/mL may be ‘inadequate’
- serum 25(OH)D >40 ng/mL is ‘sufficient’ for almost the whole population (97.5%) [101]
Testing for Vitamin D Status
Always check both forms of vitamin D; that means 25-OH and 1,25 dihydroxyvitamin (di OH). While 1,25 vitamin D is the most potent metabolite, 25-OH vitamin D levels more accurately reflect vitamin D status because parathyroid hormone and other hormones do not influence it. If you only check 25-OH after supplementing with vitamin D, and the levels don’t increase, proceed by checking the 1,25 di OH and parathyroid hormone levels. If these are either high normal or elevated out-of-range, you need to seek a professional skilled at normalizing vitamin D levels.
What is the best form of Vitamin D to be taking?
The best Vitamin D supplement is a Naturized® Whole Food Form, which contains vitamins K1 and 2 and a carotenoid complex (Red palm oil). This form is more bioavailable and effective. I use and recommend this supplement.
Naturized® whole-food nutrients are delivered in the context of a whole-food matrix that facilitates their bioavailability. This matrix includes naturally occurring peptide carriers and cofactors that act as chaperones, delivering nutrients to the cells and tissues of the body. Human physiology is designed to obtain nutrients from plants and natural foods. Naturized nutrients are designed to emulate whole foods while delivering a higher concentration of specific vitamins or minerals.
Next time you read something on the internet or hear from the mainstream news media, I suggest before you take it as gospel truth to take the advice of the Buddha.
BUDDHA SAID:
Believe nothing just because a so-called wise person said it.
Believe nothing just because a belief is generally held.
Believe nothing just because it is said in ancient books.
Believe nothing just because it is said to be of divine origin.
Believe nothing just because someone else believes it.
Believe only what you yourself test and judge to be true.
In conclusion, maintaining optimal vitamin D levels plays a crucial role in various health conditions, including cancer prevention and treatment, particularly breast cancer. Ensuring sufficient vitamin D levels through supplementation and regular testing can improve overall health and well-being.
About the Author:
Donald R. Yance is the founder of the Mederi Center. A Clinical Master Herbalist and Certified Nutritionist, Donnie is renowned for his extraordinary knowledge and deep understanding of the healing properties of plants and nutrition, as well as of epigenetics, laboratory medicine, oncologic pathology, and molecular oncology. He is a professional member of the American Herbalists Guild, National Association of Nutrition Professionals, Academy of Integrative Health and Medicine, and the Society for Integrative Oncology.
[1] Thomson CA, Aragaki AK, Prentice RL, Stefanick ML, Manson JE, Wactawski-Wende J, Watts NB, Van Horn L, Shikany JM, Rohan TE, Lane DS, Wild RA, Robles-Morales R, Shadyab AH, Saquib N, Cauley J. Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women: Postintervention Follow-up of a Randomized Clinical Trial. Ann Intern Med. 2024 Mar 12. doi: 10.7326/M23-2598. Epub ahead of print. PMID: 38467003.
[2] Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, Burckhardt P, Li R, Spiegelman D, Specker B, Orav JE, Wong JB, Staehelin HB, O’Reilly E, Kiel DP, Willett WC. Calcium intake and hip fracture risk in men and women: a meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr. 2007 Dec;86(6):1780-90. doi: 10.1093/ajcn/86.5.1780. PMID: 18065599.
[3] Zhao JG, Zeng XT, Wang J, Liu L. Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA. 2017 Dec 26;318(24):2466-2482. doi: 10.1001/jama.2017.19344. PMID: 29279934; PMCID: PMC5820727.
[4] Zach Rozenbaum, Tatsunori Takahashi, Yuhei Kobayashi, Dimitrios Bliagos, Mark Menegus, Antonio Colombo, Azeem Latib, Contemporary technologies to modify calcified plaque in coronary artery disease,
Progress in Cardiovascular Diseases, 2021, https://doi.org/10.1016/j.pcad.2021.07.003.
[5]Speer, M.Y.; Yang, H.-Y.; Brabb, T.; Leaf, E.; Look, A.; Lin, W.-L.; Frutkin, A.; Dichek, D.; Giachelli, C.M. Smooth Muscle Cells Give Rise to Osteochondrogenic Precursors and Chondrocytes in Calcifying Arteries. Circ. Res. 2009, 104, 733–741.
[6]Karwowski,W.; Naumnik, B.; Szczepa´ nski, M.; My´sliwiec, M. The mechanism of vascular calcification—A systematic review. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2012, 18, RA1–RA11.
[7] Johnson RC, Leopold JA, Loscalzo J. Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res. 2006; 99: 1044–59.
[8] Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004; 24: 1161–70.
[9] Kapustin A, Shanahan CM. Targeting vascular calcification: softening-up a hard target. Curr Opin Pharmacol. 2009; 9: 84–9.
[10] Sarnak MJ, Amann K, Bangalore S, Cavalcante JL, Charytan DM, Craig JC, Gill JS, Hlatky MA, Jardine AG, Landmesser U, Newby LK, Herzog CA, Cheung M, Wheeler DC, Winkelmayer WC, Marwick TH; Conference Participants. Chronic Kidney Disease and Coronary Artery Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019 Oct 8;74(14):1823-1838. doi: 10.1016/j.jacc.2019.08.1017. PMID: 31582143.
[11] Pijuan J, Cantarero L, Natera-de Benito D, Altimir A, Altisent-Huguet A, Díaz-Osorio Y, Carrera-García L, Expósito-Escudero J, Ortez C, Nascimento A, Hoenicka J, Palau F. Mitochondrial Dynamics and Mitochondria-Lysosome Contacts in Neurogenetic Diseases. Front Neurosci. 2022 Jan 31;16:784880. doi: 10.3389/fnins.2022.784880. PMID: 35177962; PMCID: PMC8844575.
[12] Henein M, Granåsen G, Wiklund U, Schmermund A, Guerci A, Erbel R, Raggi P. High dose and long-term statin therapy accelerate coronary artery calcification. Int J Cardiol. 2015 Apr 1;184:581-586. doi: 10.1016/j.ijcard.2015.02.072. Epub 2015 Feb 24. PMID: 25769003.
[13] Joshua Zhaojun Xian, Mimi Lu, Felicia Fong, Rong Qiao, et. al. Statin Effects on Vascular Calcification Microarchitectural Changes in Aortic Calcium Deposits in Aged Hyperlipidemic Mice, , Arterioscler Thromb Vasc Biol. 2021;41:e185–e192. DOI: 10.1161/ATVBAHA.120.315737
[14] Tanaka, N., Arima, K., Nishimura, T. et al. Vitamin K deficiency, evaluated with higher serum ucOC, was correlated with poor bone status in women. J Physiol Anthropol 39, 9 (2020). https://doi.org/10.1186/s40101-020-00221-1
[15] Urano A, Hotta M, Ohwada R, Araki M. Vitamin K deficiency evaluated by serum levels of undercarboxylated osteocalcin in patients with anorexia nervosa with bone loss. Clin Nutr. 2015 Jun;34(3):443-8. doi: 10.1016/j.clnu.2014.04.016. Epub 2014 May 28. PMID: 24909585.
[16] Shioi A, Morioka T, Shoji T, Emoto M. The Inhibitory Roles of Vitamin K in Progression of Vascular Calcification. Nutrients. 2020 Feb 23;12(2):583. doi: 10.3390/nu12020583. PMID: 32102248; PMCID: PMC7071387.
[17] van Ballegooijen AJ, Pilz S, Tomaschitz A, Grübler MR, Verheyen N. The Synergistic Interplay between Vitamins D and K for Bone and Cardiovascular Health: A Narrative Review. Int J Endocrinol. 2017;2017:7454376. doi:10.1155/2017/7454376
[18] Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. 2016 Jan;82:42-9. doi: 10.1016/j.bone.2015.05.046. Epub 2015 Jun 6. PMID: 26055108; PMCID: PMC4670816.
[19] Stock M, Schett G. Vitamin K-Dependent Proteins in Skeletal Development and Disease. Int J Mol Sci. 2021 Aug 28;22(17):9328. doi: 10.3390/ijms22179328. PMID: 34502245; PMCID: PMC8430550.
[20] Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. 2016 Jan;82:42-9. doi: 10.1016/j.bone.2015.05.046. Epub 2015 Jun 6. PMID: 26055108; PMCID: PMC4670816.
[21] Moon JS, Jin MH, Koh HM. Association between Serum Osteocalcin Levels and Metabolic Syndrome according to the Menopausal Status of Korean Women. J Korean Med Sci. 2021 Mar 1;36(8):e56. doi: 10.3346/jkms.2021.36.e56. PMID: 33650335; PMCID: PMC7921371.
[22] Guo Q, Li H, Xu L, Wu S, Sun H, Zhou B. Undercarboxylated osteocalcin reverts insulin resistance induced by endoplasmic reticulum stress in human umbilical vein endothelial cells. Sci Rep. 2017 Mar 3;7(1):46. doi: 10.1038/s41598-017-00163-2. PMID: 28246389; PMCID: PMC5427815.
[23] Fusaro M, Cianciolo G, Brandi ML, Ferrari S, Nickolas TL, Tripepi G, Plebani M, Zaninotto M, Iervasi G, La Manna G, Gallieni M, Vettor R, Aghi A, Gasperoni L, Giannini S, Sella S, M Cheung A. Vitamin K and Osteoporosis. Nutrients. 2020 Nov 25;12(12):3625. doi: 10.3390/nu12123625. PMID: 33255760; PMCID: PMC7760385.
[24] Yu Zhang, Fang Fang, professor, Jingjing Tang, doctoral student, Lu Jia, associate professor, Yuning Feng, resident, Ping Xu, associate professor, Andrew Faramand, resident, Association
between vitamin D supplementation and mortality: systematic review and meta-analysis, BMJ 2019; 366 doi: https://doi.org/10.1136/bmj.l4673 (Published 12 August 2019)
[25] Pilz S, Dobnig H, Tomaschitz A, Kienreich K, Meinitzer A, Friedl C, Wagner D, Piswanger-Sölkner C, März W, Fahrleitner-Pammer A. Low 25-hydroxyvitamin D is associated with increased mortality in female nursing home residents. J Clin Endocrinol Metab. 2012 Apr;97(4):E653-7. doi: 10.1210/jc.2011-3043. Epub 2012 Feb 8. PMID: 22319037.
[26]Serra MO, de Macedo LR, Silva M, Lautner RQ. Effect of Vitamin D supplementation on blood pressure in hypertensive individuals with hypovitaminosis D: a systematic review and meta-analysis. J Hypertens. 2024 Apr 1;42(4):594-604. doi: 10.1097/HJH.0000000000003646. Epub 2023 Dec 18. PMID: 38164948.
[27] Saliba W, Barnett O, Rennert HS, Rennert G. The risk of all-cause mortality is inversely related to serum 25(OH)D levels. J Clin Endocrinol Metab. 2012 Aug;97(8):2792-8. doi: 10.1210/jc.2012-1747. Epub 2012 May 30. PMID: 22648653.
[28]Eirik Degerud, Ottar Nygård, Stefan de Vogel, Rune Hoff, Gard Frodahl Tveitevåg Svingen, Eva Ringdal Pedersen, Dennis Winston Trygve Nilsen, Jan Erik Nordrehaug, Øivind Midttun, Per Magne Ueland, Jutta Dierkes. Plasma 25-hydroxyvitamin D and mortality in patients with suspected stable angina pectoris. The Journal of Clinical Endocrinology & Metabolism, 2018; DOI: 10.1210/jc.2017-02328
[29] Cubbon RM, Lowry JE, Drozd M, Hall M, Gierula J, Paton MF, Byrom R, Kearney LC, Barth JH, Kearney MT, Witte KK. Vitamin D deficiency is an independent predictor of mortality in patients with chronic heart failure. Eur J Nutr. 2019 Sep;58(6):2535-2543. doi: 10.1007/s00394-018-1806-y. Epub 2018 Aug 18. PMID: 30121806; PMCID: PMC6689317.
[30]Zhao G, Ford ES, Li C, Croft JB. Serum 25-hydroxyvitamin D levels and all-cause and cardiovascular disease mortality among US adults with hypertension: the NHANES linked mortality study. J Hypertens. 2012 Feb;30(2):284-9. doi: 10.1097/HJH.0b013e32834e1f0a. PMID: 22179077.
[31]Sood A, Arora R., Vitamin D Deficiency and Its Correlations With Increased Cardiovascular
Incidences, Am J Ther. 2009 May 15.
[32]Morioka TY, Lee AJ, Bertisch S, Buettner C. Vitamin D status modifies the association between statin use and musculoskeletal pain: a population based study. Atherosclerosis. 2015 Jan;238(1):77-82. doi: 10.1016/j.atherosclerosis.2014.11.012. Epub 2014 Nov 20. PMID: 25437894; PMCID: PMC4277894.
[33]Wang H, Chen W, Li D, Yin X, Zhang X, Olsen N, Zheng SG. Vitamin D and Chronic Diseases. Aging Dis. 2017 May 2;8(3):346-353. doi: 10.14336/AD.2016.1021. PMID: 28580189; PMCID: PMC5440113.
[34] Menon V, Kar SK, Suthar N, Nebhinani N. Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian J Psychol Med. 2020 Jan 6;42(1):11-21. doi: 10.4103/IJPSYM.IJPSYM_160_19. PMID: 31997861; PMCID: PMC6970300.
[35] Anglin RES, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. British Journal of Psychiatry. 2013;202(2):100-107. doi:10.1192/bjp.bp.111.106666
[36] Sîrbe C, Rednic S, Grama A, Pop TL. An Update on the Effects of Vitamin D on the Immune System and Autoimmune Diseases. Int J Mol Sci. 2022 Aug 29;23(17):9784. doi: 10.3390/ijms23179784. PMID: 36077185; PMCID: PMC9456003.
[37] Ao T, Kikuta J, Ishii M. The Effects of Vitamin D on Immune System and Inflammatory Diseases. Biomolecules. 2021 Nov 3;11(11):1624. doi: 10.3390/biom11111624. PMID: 34827621; PMCID: PMC8615708.
[38]Md Isa Z, Amsah N, Ahmad N. The Impact of Vitamin D Deficiency and Insufficiency on the Outcome of Type 2 Diabetes Mellitus Patients: A Systematic Review. Nutrients. 2023 May 15;15(10):2310. doi: 10.3390/nu15102310. PMID: 37242192; PMCID: PMC10223393.
[39] Sultan S, Taimuri U, Basnan SA, Ai-Orabi WK, Awadallah A, Almowald F, Hazazi A. Low Vitamin D and Its Association with Cognitive Impairment and Dementia. J Aging Res. 2020 Apr 30;2020:6097820. doi: 10.1155/2020/6097820. PMID: 32399297; PMCID: PMC7210535.
[40] De Martinis M, Allegra A, Sirufo MM, Tonacci A, Pioggia G, Raggiunti M, Ginaldi L, Gangemi S. Vitamin D Deficiency, Osteoporosis and Effect on Autoimmune Diseases and Hematopoiesis: A Review. Int J Mol Sci. 2021 Aug 17;22(16):8855. doi: 10.3390/ijms22168855. PMID: 34445560; PMCID: PMC8396272.
[41] Vellingiri K, Ethiraj P, S NJ, Shanthappa AH, J KS. Assessment of Vitamin D Levels and Its Correlation With Osteoporosis and Fracture Site Comminution in Osteoporotic Hip Fractures in Tertiary Care Hospital. Cureus. 2021 Jan 29;13(1):e12982. doi: 10.7759/cureus.12982. PMID: 33654639; PMCID: PMC7916318.
[42]Seraphin G, Rieger S, Hewison M, Capobianco E, Lisse TS. The impact of vitamin D on cancer: A mini review. J Steroid Biochem Mol Biol. 2023 Jul;231:106308. doi: 10.1016/j.jsbmb.2023.106308. Epub 2023 Apr 11. PMID: 37054849; PMCID: PMC10330295.
[43]Despoina Manousaki, Brent Richards, et. al., Low vitamin D levels as a risk factor for cancer, BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j4952 (Published 31 October 2017)Cite this as: BMJ 2017;359:j4952
[44] Michelle R. Hoffmann, Peter A. Senior, Diana R. Mager, Vitamin D Supplementation and Health-Related Quality of Life: A Systematic Review of the Literature,Journal of the Academy of Nutrition and Dietetics,Volume 115, Issue 3, 2015, Pages 406-418,ISSN 2212-2672, https://doi.org/10.1016/j.jand.2014.10.023.
[45]Manoy P, Yuktanandana P, Tanavalee A, Anomasiri W, Ngarmukos S, Tanpowpong T, Honsawek S. Vitamin D Supplementation Improves Quality of Life and Physical Performance in Osteoarthritis Patients. Nutrients. 2017 Jul 26;9(8):799. doi: 10.3390/nu9080799. PMID: 28933742; PMCID: PMC5579593.
[46] Sobhi P, Bahrami M, Mahdizadeh F, Fazaeli A, Babaei G, Rezagholizadeh L. Vitamin D and potential effects on cancers: a review. Mol Biol Rep. 2024 Jan 25;51(1):190. doi: 10.1007/s11033-023-09111-y. PMID: 38270702.
[47] Keum N, Chen QY, Lee DH, Manson JE, Giovannucci E. Vitamin D supplementation and total cancer incidence and mortality by daily vs. infrequent large-bolus dosing strategies: a meta-analysis of randomised controlled trials. Br J Cancer. 2022 Sep;127(5):872-878. doi: 10.1038/s41416-022-01850-2. Epub 2022 Jun 8. PMID: 35676320; PMCID: PMC9427835.
[48] Keum N, Lee DH, Greenwood DC, Manson JE, Giovannucci E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Ann Oncol. 2019 May 1;30(5):733-743. doi: 10.1093/annonc/mdz059. PMID: 30796437; PMCID: PMC6821324.
[49]Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, Lipkin M, et al. (2005). Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol, 97: 179-194
[50]Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, et al. (2006). The role of vitamin D in cancer prevention. Am J Public Health, 96: 252-261
[51]Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP (2007). Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr, 85: 1586-1591
[52] Sha S, Chen LJ, Brenner H, Schöttker B. Associations of 25-hydroxyvitamin D status and vitamin D supplementation use with mortality due to 18 frequent cancer types in the UK Biobank cohort. Eur J Cancer. 2023 Sep;191:113241. doi: 10.1016/j.ejca.2023.113241. Epub 2023 Jul 17. PMID: 37549530.
[53]Murphy, A.B., Vitamin D Deficiency Linked to Aggressive Prostate Cancer, American Association for Cancer Research, Northwestern University Feinberg School of Medicine, Chicago, Illinois | DG News 5/1/14, 2:41 PM http://dgnews.docguide.com/vitamin-d-deficiency-linked-aggressive-prostate cancer?overlay=2&nl_ref=newsletter&pk_campaign=newsletter Page 3 of 3
[54] Kanaan, Y., Copeland, R.L. The link between vitamin D and prostate cancer. Nat Rev Cancer 22, 435 (2022). https://doi.org/10.1038/s41568-022-00493-y
[55]Wang JY, Swami S, Krishnan AV, Feldman D. Combination of calcitriol and dietary soy exhibits enhanced anticancer activity and increased hypercalcemic toxicity in a mouse xenograft model of prostate cancer. Prostate. 2012 Mar 27. doi: 10.1002/pros.22516.
[56]Giovannucci E. Dietary influences of 1,25(OH)2 vitamin D in relation to prostate cancer: a hypothesis. Cancer Causes Control. 1998;9:567-582.
[57]Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, Holick MF. The role of vitamin D in cancer prevention. Am J Public Health. 2006 Feb;96(2):252-61. Epub 2005 Dec 27.
[58]Giovannucci, Dr. Edward, Hypovitaminosis D: a Modifiable Cancer Risk Factor in Black Men? Cancer Epidemiol Biomarkers Prev, December, 2006;15:2467-2472.
[59]Peehl DM et al . (2003) Pathways mediating the growth-inhibitory actions of vitamin D in prostate cancer. J Nutr 133: 2461S-2469S.
[60] Krishnan AV et al . (2003) Inhibition of prostate cancer growth by vitamin D: regulation of target gene expression. J Cell Biochem 88: 363-371.
[61]Beer TM, Myrthue A, Garzotto M, O’hara MF, Chin R, Lowe BA, Montalto MA, Corless CL, Henner WD. Randomized study of high-dose pulse calcitriol or placebo prior to radical prostatectomy. Cancer Epidemiol Biomarkers Prev. 2004 Dec;13(12):2225-32.
[63] Palmieri C, Macgregor T, Girgis S, Vigushin D. Serum 25 hydroxyvitamin D levels in early and advanced breast cancer. J Clin Pathol. 2006 Oct 17
[64]Katie M. O’Brien PhD,Quaker E. Harmon MD, PhD,Chandra L. Jackson PhD,Mary V. Diaz-Santana PhD, et. al., Vitamin D concentrations and breast cancer incidence among Black/African American and non-Black Hispanic/Latina women, First published: 25 April 2022, https://doi.org/10.1002/cncr.34198
[65]Crew KD, Gammon MD, Steck SE, Hershman DL, Cremers S, Dworakowski E, Shane E, Terry MB, Desai M, Teitelbaum SL, NeugutAI, Santella RM. Association between Plasma 25-Hydroxyvitamin D and Breast Cancer Risk, Cancer Prev Res (Phila Pa). 2009 May 26.
[66]Kim, Y., Kim Je., Vitamin D intake, blood 25(OH)D levels, and breast cancer risk or mortality: a meta-analysis, Br J Cancer. 2014 May 27; 110(11): 2772–2784, Published online 2014 Apr 8. doi: 10.1038/bjc.2014.175
[67]Kim JA, Choi R, Won H, Kim S, Choi HJ, Ryu JM, Lee SK, Yu J, Kim SW, Lee JE, Lee SY. Serum Vitamin Levels and Their Relationships with Other Biomarkers in Korean Breast Cancer Patients. Nutrients. 2020 Sep 16;12(9):E2831. doi: 10.3390/nu12092831. PMID: 32947849.
[68]Li Laine Ooi, Hong Zhou, Robert Kalak, Yu Zheng, Arthur D. Conigrave, Markus J. Seibel and Colin R. Dunstan, Vitamin D Deficiency Promotes Human Breast Cancer Growth in a Murine Model of Bone Metastasis, Cancer Res;70(5); 1835–44
[69] Morrison, Alex, Vitamin D Supplementation Improves Outcomes in Women With HER2-Positive Breast Cancer, SAN ANTONIO, Tex – December 17, 2013, [Presentation title: Improved Clinical Outcomes Associated With Vitamin D Supplementation During Adjuvant Chemotherapy in Patients With HER2+ Non-Metastatic Breast Cancer. Abstract P609-02]
[70]Chen CS, Zirpoli G, Barlow WE, et al. Vitamin D insufficiency as a risk factor for paclitaxel-induced peripheral neuropathy in SWOG S0221. J Natl Compr Canc Netw. 2023;21(11):1172-1180.e3. doi:10.6004/jnccn.2023.7062
[71] Zheng W, Peng W, Qian F, Zhang M, Duan B, Fan Z, Xie Y, Fu X. Vitamin D suppresses CD133+/CD44 + cancer stem cell stemness by inhibiting NF-κB signaling and reducing NLRP3 expression in triple-negative breast cancer. Cancer Chemother Pharmacol. 2024 Mar 8. doi: 10.1007/s00280-024-04660-w. Epub ahead of print. PMID: 38456956.
[72]Lina Zgaga, Evropi Theodoratou, Susan M. Farrington, Farhat V.N. Din, Li Yin Ooi, Dominik Glodzik, Susan Johnston, Albert Tenesa, Harry Campbell and Malcolm G. Dunlop, Plasma Vitamin D Concentration Influences Survival Outcome After a Diagnosis of Colorectal Cancer, JCO JCO.2013.54.5947; published online on July 7, 2014
[73]Kimmie Ng, MD, MPH; Halla S. Nimeiri, MD; Nadine J. McCleary, MD, MPH, Thomas A. Abrams, MD; et. al.; Effect of High-Dose vs Standard-Dose Vitamin D3 Supplementation on Progression-Free Survival Among Patients With Advanced or Metastatic Colorectal Cancer, The SUNSHINE Randomized Clinical Trial, April 19, 2019, JAMA. 2019;321(14):1370-1379. doi:10.1001/jama.2019.2402.
[74] Kim H, Lipsync-Sharf M, Zong X, et al. Total vitamin D intake and risks of early-onset colorectal cancer and precursors. Gastroenterology. Published online July 7, 2021. doi:10.1053/j.gastro.2021.07.002
[75] Akutsu, T.; Kitamura, H.; Himeiwa, S.; Kitada, S.; Akasu, T.; Urashima, M. Vitamin D and Cancer Survival: Does Vitamin D Supplementation Improve the Survival of Patients with Cancer? Curr. Oncol. Rep. 2020, 22, 62.
[76]Galus Ł, Michalak M, Lorenz M, Stoińska-Swiniarek R, Tusień Małecka D, Galus A, Kolenda T, Leporowska E, Mackiewicz J. Vitamin D supplementation increases objective response rate and prolongs progression-free time in patients with advanced melanoma undergoing anti-PD-1 therapy. Cancer. 2023 Jul 1;129(13):2047-2055. doi: 10.1002/cncr.34718. Epub 2023 Apr 24. PMID: 37089083.
[77] Shokri-Mashhadi N, Kazemi M, Saadat S, Moradi S. Effects of select dietary supplements on the prevention and treatment of viral respiratory tract infections: a systematic review of randomized controlled trials. Expert Rev Respir Med. 2021 Apr 26:1-17. doi: 10.1080/17476348.2021.1918546. Epub ahead of print. PMID: 33858268.
[78] Dror, Amiel A et al. “Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness.” PloS one vol. 17,2 e0263069. 3 Feb. 2022, doi:10.1371/journal.pone.0263069
[79] Meltzer DO, Best TJ, Zhang H, Vokes T, Arora VM, Solway J. Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results. JAMA Netw Open. 2021;4(3):e214117. doi:10.1001/jamanetworkopen.2021.4117
[80] Corrigendum to Kazemi et al. Association of vitamin D status with SARS-COV-2 infection or COVID-19 severity: a systematic review and meta-analysis. Adv Nutr 2021;12(5):1636-58. Adv Nutr. 2021 Oct 1;12(5):2040-2044. doi: 10.1093/advances/nmab090. Erratum for: Adv Nutr. 2021 Oct 1;12(5):1636-1658. PMID: 34595506; PMCID: PMC8483944.
[81] Baktash V, Hosack T, Patel N, Shah S, Kandiah P, Van den Abbeele K, Mandal AKJ, Missouris CG. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad Med J. 2021 Jul;97(1149):442-447. doi: 10.1136/postgradmedj-2020-138712. Epub 2020 Aug 27. PMID: 32855214; PMCID: PMC7456620.
[82] Bakaloudi DR, Chourdakis M. A critical update on the role of mild and serious vitamin D deficiency prevalence and the COVID-19 epidemic in Europe. Nutrition. 2021 Jul 30;93:111441. doi: 10.1016/j.nut.2021.111441. Epub ahead of print. PMID: 34492624; PMCID: PMC8321689.
[83] Sunnetcioglu A, Sunnetcioglu M, Gurbuz E, Bedirhanoglu S, Erginoguz A, Celik S. Serum 25(OH)D Deficiency and High D-Dimer Levels are Associated with COVID-19 Pneumonia. Clin Lab. 2021 Jul 1;67(7). doi: 10.7754/Clin.Lab.2020.201050. PMID: 34258973.
[84] Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA Netw Open. 2020;3(9):e2019722. doi:10.1001/jamanetworkopen.2020.19722
[85]Dror, Amiel A et al. “Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness.” PloS one vol. 17,2 e0263069. 3 Feb. 2022, doi:10.1371/journal.pone.0263069
[86] Villasis-Keever MA, Lopez-Alarcon MG, Miranda-Novales G, et al. Efficacy and Safety of Vitamin D Supplementation to Prevent COVID-19 in Frontline Healthcare Workers. A Randomized Clinical Trial. Archives of medical research 2022;53(4):423–30. doi: 10.1016/j.arcmed.2022.04.003 [published Online First: 2022/04/30]
[87] Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, Qin Z, Peng X, Xiao H, Chen C, Liu X, Ning L, Wang B, Tang N, Li M, Xu F, Lin S, Yang J. Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study. J Am Coll Nutr. 2020 Oct 13:1-8. doi: 10.1080/07315724.2020.1826005. Epub ahead of print. PMID: 33048028.
[88] Cicero AFG, Fogacci F, Borghi C. Vitamin D Supplementation and COVID-19 Outcomes: Mounting Evidence and Fewer Doubts. Nutrients. 2022 Aug 31;14(17):3584. doi: 10.3390/nu14173584. PMID: 36079842.
[89] Athanassiou L, Kostoglou-Athanassiou I, Nikolakopoulou S, Konstantinou A, Mascha O, Siarkos E, Samaras C, Athanassiou P, Shoenfeld Y. Vitamin D Levels as a Marker of Severe SARS-CoV-2 Infection. Life (Basel). 2024 Jan 31;14(2):210. doi: 10.3390/life14020210. PMID: 38398719; PMCID: PMC10890332.
[90] Shi YY, Liu TJ, Fu JH, et al. Vitamin D/VDR signaling attenuates lipopolysaccharide‑induced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier. Mol Med Rep. 2016;13(2):1186‐1194. doi:10.3892/mmr.2015.4685
[91] Gorman S, Buckley AG, Ling KM, et al. Vitamin D supplementation of initially vitamin D-deficient mice diminishes lung inflammation with limited effects on pulmonary epithelial integrity. Physiol Rep. 2017;5(15):e13371. doi:10.14814/phy2.13371
[92] Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12(4):E988. Published 2020 Apr 2. doi:10.3390/nu12040988
[93] Heidari H, Abbasi K, Feizi A, Kohan S, Amani R. Effect of vitamin D supplementation on symptoms severity in vitamin D insufficient women with premenstrual syndrome: A randomized controlled trial. Clin Nutr ESPEN. 2024 Feb;59:241-248. doi: 10.1016/j.clnesp.2023.11.014. Epub 2023 Dec 10. PMID: 38220382.
[94]Newmark HL, Newmark J. Vitamin D and Parkinson’s disease–a hypothesis. Mov Disord. 2007 Mar 15;22(4):461-8. doi: 10.1002/mds.21317. PMID: 17230473.;
[95]Liu Y, Li YW, Tang YL, Liu X, Jiang JH, Li QG, Yuan JY. Vitamin D: preventive and therapeutic potential in Parkinson’s disease. Curr Drug Metab. 2013 Nov;14(9):989-93. doi: 10.2174/1389200211314090005. PMID: 24160295.
[96]Ascherio A, Munger KL, White R. et al. Vitamin D as an Early Predictor of Multiple Sclerosis Activity and Progression. JAMA Neurol. 2014 Jan 20. doi: 10.1001/jamaneurol.2013.5993
[97]Keane JT, Elangovan H, Stokes RA, Gunton JE. Vitamin D and the Liver-Correlation or Cause? Nutrients. 2018 Apr 16;10(4):496. doi: 10.3390/nu10040496. PMID: 29659559; PMCID: PMC5946281.
[98]H. A. Bischoff-Ferrari, W. C. Willett, J. B. Wong, et al. Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med. (2009); 169:551-61.
[99] Jagelavičienė E, Vaitkevičienė I, Šilingaitė D, Šinkūnaitė E, Daugėlaitė G. The Relationship between Vitamin D and Periodontal Pathology. Medicina (Kaunas). 2018 Jun 12;54(3):45. doi: 10.3390/medicina54030045. PMID: 30344276; PMCID: PMC6122115.
[100] Botelho J, Machado V, Proença L, Delgado AS, Mendes JJ. Vitamin D Deficiency and Oral Health: A Comprehensive Review. Nutrients. 2020 May 19;12(5):1471. doi: 10.3390/nu12051471. PMID: 32438644; PMCID: PMC7285165.
[101] Spiro A, Buttriss JL. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39(4):322‐350. doi:10.1111/nbu.12108


Thank you so much for you help,
Thank you, Donnie Yance for this life-saving information . Once again, you dispel MIS-INFORMATION. You are a blessing in the field pf health.