A silent crisis has emerged after the global COVID-19 pandemic, affecting many survivors long after their initial recovery. Long COVID, a term used to describe the lingering and debilitating symptoms experienced by individuals weeks and even months after their acute infection, has become a pressing concern in healthcare. In the face of this prolonged health crisis, a beacon of hope emerges in the form of adaptogens—natural substances with the potential to offer relief and support for those recovering from the debilitating grip of long COVID. Leveraging the power of adaptogens can unlock long COVID recovery.
Before delving into the transformative power of adaptogens, it is essential to comprehend the gravity of the issue and the urgent need for effective solutions in the realm of long COVID recovery.
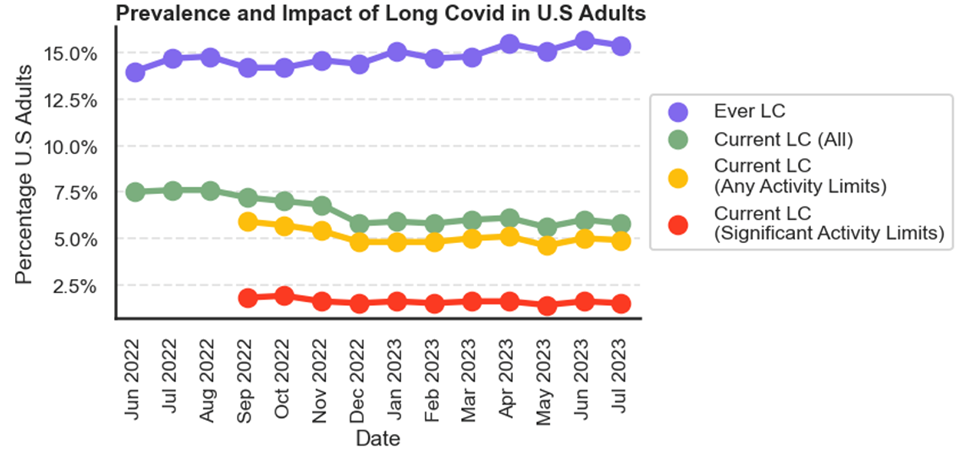
Astonishingly, even after two or more years from the onset of the initial infection, the persistence of long COVID continues to impact lives. Recent statistics paint a concerning picture: 4.9% of U.S. adults report limitations in their daily activities, and 1.5% grapple with significant restrictions for an extended period following their encounter with COVID-19.[1]
For instance, severe and unexplained fatigue, memory loss, and various neurological disorders feature prominently among the haunting array of symptoms. Moreover, an extensive study of healthcare databases reveals that those once hospitalized due to COVID-19 are likelier to endure these symptoms well beyond the one-year mark. [3]
As of the 21st of February, 2023, over 757 million confirmed cases of COVID-19, including 6.8 million deaths, were reported to the WHO [4], and approximately 43% of cases globally continue to suffer various symptoms after recovering from COVID-19.[5]
Long COVID: A Persistent and Prevalent Challenge
In recent studies, it has been suggested that many long COVID symptoms may resolve within a year. However, understanding the full scope of the issue is crucial. Fatigue, a predominant long COVID symptom, has not been thoroughly studied despite its prominence.[6]
The latest CDC data reveals that just over 15% of U.S. adults have experienced long COVID, with about 5.8% (approximately 15 million) currently grappling with it. [7]
Intriguingly, millions of Americans were exposed to SARS-CoV-2 during the pandemic but never tested positive. Now, they exhibit symptoms resembling long COVID, falling under post-viral syndrome (PVS). Sadly, many individuals are overlooked in long COVID clinics and research studies because they lack a positive test result, leaving them without specialized care.
“Since most long COVID clinics are only accepting patients with a positive test result, these people experiencing identical symptoms are left without specialized care and excluded from research studies on long COVID,” according to Igor J. Koralnik, M.D., chief of neuro-infectious disease and global neurology in the Department of Neurology at Northwestern Medicine Comprehensive COVID-19 Center in Chicago.
Additionally, a study conducted by Dr. Koralnik and a team of researchers found that patients with post-viral syndrome experienced quality-of-life impairments, including declines in cognitive function and increases in fatigue.[8]
Despite the availability of vaccines, there’s still a concerning rise in morbidity and post-COVID-19 conditions. As highlighted in extensive retrospective cohort studies, new autoimmune and inflammatory diseases emerge among those with the virus.[9]
COVID-Induced Neurological Disorders
A systematic review and meta-analysis showed that patients who recovered from COVID-19 had lower general cognition compared to healthy controls up to 7 months post-infection.[10]
COVID-19 may trigger complex biological reactions from the gut to the brain, leading to persistent neurological symptoms in some people. According to new research, a subset of long COVID patients develop chronic neuroinflammation that interferes with a key chemical messenger involved in nerve activity, brain function, and memory.[11]
Certainly, the impact of COVID-19 on the nervous system can be attributed to various potential mechanisms. At least four distinct pathways may explain the negative effects of the virus on the nervous system:
1) Direct viral encephalitis
2) Systemic inflammation
3) Peripheral organ dysfunction (liver, kidney, lung, etc.)
4) Cerebrovascular changes[12]
Adaptogen Can Help People Recovering from Long COVID
Adaptogens, a category of plants known for supporting the body’s networks and promoting homeostasis, are crucial in long COVID recovery and revitalization. [13] These natural remedies, embraced in traditional medicine worldwide, enhance energy levels, combat stress, and restore balance. Referred to as restoratives, qi-tonics, or rejuvenating herbs, adaptogens have been revered for centuries. They play a vital role in traditional healing systems, particularly in traditional Chinese medicine, where tonic herbs are highly prized.
According to a recent systematic review and meta-analysis published study in the October 2023 issue of Therapeutic Advances in Chronic Disease,[14] holistic medicine interventions, specifically self-administered vagus nerve stimulation, neuro-meditation, herbal and nutritional supplements, aromatherapy, have shown some promising results for people experiencing long COVID.
Activation of the vagus nerve, which innervates internal organs, stimulating neurons in the hippocampus, leads to improved memory and cognition.[15]
A Network of Interactions
These adaptogenic formulations impact biological networks and influence their interactions, ranging from genes and proteins to cells and organ systems, reinforcing overall health and well-being. For more on this, read my blog, “Adaptogens, Bioregulatory Systems Medicine and Network Pharmacology.”
Adaptogens Expand the Body’s Dynamic Range of Equilibrium
When a system operates in a state of “dynamic equilibrium,” there is a level of tension between opposing forces that is healthy, intentional, and designed to achieve maximum results.[16]
When an organism is pushed outside of this equilibrium, diseases can do harm. Adaptogenic herbs expand the dynamic range of equilibrium in which the organism operates.
The output dynamics of one system can be affected by changes in the dynamics of other systems. This is what I mean by “a network of interactions”. For example, there are 33 human proteins involved in converting carbohydrates into fuel and 830 interactions with metabolites.[17]
Only plant intelligence, herbal, and dietary medicine can communicate with all these network interactions, lending a helping hand throughout.
Traditional herbal medicine is usually made up of various formulas comprising multiple herbs in a single formula.
The formulas show their clinical effects by playing critical therapeutic roles through “multi-component, multi-target and multi-pathway” mechanisms.[18]
How Adaptogens Fight Off Viral Infections and Aid in Recovery
The evidence from pre-clinical and clinical studies with adaptogens such as Eleutherococcus senticosus, Panax ginseng, Rhodiola rosea, Schisandra chinensis, Withania somnifera, and licorice (Glycyrrhiza spp.) show that adaptogens can be useful in preventing and treating viral infections at all stages of progression of inflammation. They can also help aid recovery. Adaptogens do this by:
1) modulating innate and adaptive immunity,
2) anti-inflammatory activity,
3) detoxification and repair of oxidative stress-induced damage in compromised cells,
4) direct antiviral effects of inhibiting viral docking or replication and
5) improving quality of life during convalescence.[19]
Severe Long COVID-19 Is Linked to A Dysregulated Immune System, Chronic Inflammation, and Increased Risk for Autoimmune Disease
Viral infections triggering autoimmune conditions have intrigued scientists for years. Increasing evidence points to COVID-19 causing immune system dysregulation and the emergence of autoimmune phenomena.
A study in Cell indicates that severe COVID-19 can lead to lasting changes in the innate immune system. Researchers observed epigenetic modifications in stem cells of COVID-19 patients requiring intubation and ventilation, resulting in higher levels of inflammatory molecules like cytokines. [20] Notably, elevated interleukin-6 (IL-6) levels are linked to long COVID, contributing to persistent symptoms. [21]
These cellular changes persist for up to a year after infection, potentially explaining the widespread organ damage seen in COVID-19 and the high inflammation levels in long COVID patients, as reported by the National Institutes of Health.[22]
Cytokine NLRP3
Many of the long COVID conditions relate to a specific cytokine called NLRP3 inflammasome. The NLRP3 inflammasome, activating IL-1β, plays a role in prolonged inflammation, leading to respiratory issues, hypercoagulability, and autoimmune disorders.[23] This cytokine becomes overexpressed and doesn’t normalize after the acute infection has subsided.
Adaptogens, such as Panax ginseng, are potential regulators of the NLRP3 inflammasome.[24]
Triggering Pleiotropy
Adaptogens trigger pleiotropic genes, molecular mechanisms, and cellular signaling pathways mediating adaptive and defense responses. This results in simultaneously multitarget modes of action and nonspecific pleiotropic pharmacological activity.
Pleiotropy is the result of the effect of adaptogens on a single gene that impacts multiple signaling pathways, biological processes, physiological functions, and phenotype characteristics.
Various cells use the gene transcription mechanism that triggers numerous downstream signaling pathways and molecular networks that collectively affect multiple molecular targets, resulting in many pharmacological activities collectively considered nonspecific effects.[25]
Neuroprotective Effects
Adaptogens exhibit neuroprotective effects, and dozens of clinical studies have found that they increase cognitive function.
For example, one study discovered that adaptogenic extracts significantly attenuated cytostatic-induced regulation of more than 100 genes involved in activating neuronal death and inhibiting neurogenesis.[26]
The most extensively studied adaptogens for treating mental and behavioral disorders are Eleutherococcus senticosus, Rhodiola rosea, and Schisandra chinensis. According to a 15-page scientific paper published by a Swedish researcher in 2013, these adaptogens can help treat stress-induced fatigue, chronic fatigue, depression, neurosis, bipolar disorder, and even schizophrenia.[27]
There is a large body of evidence that indicates neuroprotective effects of Eleutherococcus.[28] Eleutherococcus senticosus is often called the king of adaptogenic plants.
Adaptogens Immune-potentiating Activity
Adaptogens’ immune-potentiating activity is believed to be mediated by modulation of T-cell immunity biochemical factors, transcription factors, some genes and factors associated with tumor development and progression.
Combining active immune-stimulating constituents from these plants may provide even better homeostasis than any one plant. As one 2017 study found, these immunological factors suggest their potential therapeutic significance in adjuvant or supportive therapy in cancer treatment and other immune disorders.[29]
Adaptogens in Patients with Long COVID: A Randomized, Quadruple-Blind, Placebo-Controlled Trial
In March of 2022, the National Library of Medicine published an interesting and well-designed study. This involved a randomized, quadruple-blind, placebo-controlled scientific study to assess adaptogens’ efficacy on patients recovering from long COVID.
The researchers included 100 patients with confirmed positive SARS-CoV-2 tests who experienced long COVID symptoms 30 days before randomization.
Those recovering from long COVID experienced at least three of the following nine symptoms:
Cognitive issues
Coughing
Fatigue
Headache
Loss of smell, taste, or hair
Mood disorders
Pain in their joints, muscles, or chest
Respiratory insufficiency
Sweatiness
This study, conducted by a large international team of scientists, examined the efficacy of ADAPT-232.
ADAPT-232 is a fixed combination of adaptogens Rhodiola, Eleutherococcus, and Schisandra. The supplementation lasted two weeks.
Less Pain, Less Fatigue
In 50% of the patients, ADAPT-232 decreased the duration of fatigue and pain for one and two days, respectively.
On Days 9 and 11, the number of patients with a lack of fatigue and pain symptoms was significantly less in the ADAPT-232 treatment group than in the placebo group.
In addition, ADAPT-232 significantly decreased blood creatinine compared to the placebo. This suggests it can prevent renal failure progression in patients recovering from long COVID.[30]
My Philosophy of Healing
My healing philosophy centers on the intricate interplay of the body’s network systems and the ongoing balance between breaking down (catabolism) and building up (anabolism). A key element of my approach includes incorporating adaptogenic herbs and immunonutrients. These support anabolic metabolism, aiding in the holistic development of the body. I firmly believe nurturing a person’s vital force is paramount in healing.
Basic clinical concepts that must always be addressed when treating a patient recovering from long COVID include the following:
• Enhance vitality and adaptive capability by strengthening the person in a rational and nontoxic fashion
• Balance the endocrine and nervous systems
• Improve metabolism, digestion, and assimilation
• Activate the body’s innate healing mechanisms by taking notice of the blood, lymph, liver, kidneys, bowels, lungs, and skin to assess where detoxification is needed
• Address imbalances and deficiencies with specifically indicated remedies
• Use adaptogenic formulations to build up and support innate immunity
Combinations Work Better Than Single Herbs
I never use single adaptogens or herbs. A combination of adaptogenic plants provides unique effects due to their synergistic interactions not obtainable by any ingredient independently.
Complex herbal mixtures represent smart combination therapies of hundreds or more compounds that decrease the risk of resistance development and exert unitive interactions.
Although I customize an individualized protocol for each person I see, some foundational formulas benefit almost everyone who comes to me. I use two main adaptogenic formulas: One comprises a combination of primary, secondary, and companion adaptogens, providing a well-rounded, balanced formula suitable for anyone who desires to reduce stress and achieve optimal health.
Tradtional and Modern
The herbs included are highly revered both as traditional tonics used throughout the world (up to thousands of years in Traditional Chinese Medicine and Ayurvedic Medicine) and as herbs that have an enormous amount of recent scientific research that validates their historical usage and gives us new insights into their overall benefits.
The second formula comprises primary adaptogens only and is more specific for energy and endurance.
These two formulas immediately benefit people after acute COVID-19 has subsided. I double the dosage for a short period, perhaps 2 to 4 weeks, to help with recovery for anyone recovering from COVID-19 or another infection or any increased stress on their immune system or other organ system of the body.
Over the past forty years of helping people restore vitality and optimize their health, I’ve found these formulations to be the most effective.
For more information on the importance of adaptogens in human health, please read my book, Adaptogens in Medical Herbalism.
About the Author:
Donald R. Yance is the founder of the Mederi Center. A Clinical Master Herbalist and Certified Nutritionist, Donnie is renowned for his extraordinary knowledge and deep understanding of the healing properties of plants and nutrition, as well as of epigenetics, laboratory medicine, oncologic pathology, and molecular oncology. He is a professional member of the American Herbalists Guild, National Association of Nutrition Professionals, Academy of Integrative Health and Medicine, and the Society for Integrative Oncology.
[1] Bonuck, Karen PhD July 23, 2023, Long COVID Persists as a Mass Disabling Event, MEDPAGETODAY, https://www.medpagetoday.com/opinion/second-opinions/105599?xid=nl_mpt_DHE_2023-07-29&eun=g1065123d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=Weekly%20Review%202023-07-29&utm_term=NL_DHE_Weekly_Active
[2] Rahmati M, Udeh R, Yon DK, Lee SW, Dolja-Gore X, McEVoy M, Kenna T, Jacob L, López Sánchez GF, Koyanagi A, Shin JI, Smith L. A systematic review and meta-analysis of long-term sequelae of COVID-19 2-year after SARS-CoV-2 infection: A call to action for neurological, physical, and psychological sciences. J Med Virol. 2023 Jun;95(6):e28852. doi: 10.1002/jmv.28852. PMID: 37288652.
[3] Harris E. Some People Still Have Long COVID Symptoms After 2 Years. JAMA. Published online September 06, 2023. doi:10.1001/jama.2023.16677
[4] WHO. WHO coronavirus (COVID-19) dashboard, https://covid19.who.int/ (2022, accessed 29 December 2022).
[5] Chen C, Haupert SR, Zimmermann L, et al. Global prevalence of post COVID-19 condition or long COVID: a meta-analysis and systematic review. J Infect Dis 2022; 226: 1593–1607.
[6] Mizrahi B, Sudry T, Flaks-Manov N, Yehezkelli Y, Kalkstein N, Akiva P, Ekka-Zohar A, Ben David SS, Lerner U, Bivas-Benita M, Greenfeld S. Long covid outcomes at one year after mild SARS-CoV-2 infection: nationwide cohort study. BMJ. 2023 Jan 11;380:e072529. doi: 10.1136/bmj-2022-072529. PMID: 36631153; PMCID: PMC9832503.
[7] https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm
[8] Orban ZS, Visvabharathy L, Perez Giraldo GS, Jimenez M, Koralnik IJ. SARS-CoV-2-specific immune responses in patients with postviral syndrome after suspected COVID-19. Neurol Neuroimmunol Neuroinflamm. 2023;10(6):e200159. Published online August 23, 2023. doi:10.1212/NXI.0000000000200159
[9] Chang, R. et al. Risk of autoimmune diseases in patients with COVID-19: A retrospective cohort study. eClinicalMedicine 56, 101783 (2023).
[10] Crivelli L, Palmer K, Calandri I, Guekht A, Beghi E, Carroll W, Frontera J, García-Azorín D, Westenberg E, Winkler AS, Mangialasche F, Allegri RF, Kivipelto M. Changes in cognitive functioning after COVID-19: A systematic review and meta-analysis. Alzheimers Dement. 2022 May;18(5):1047-1066. doi: 10.1002/alz.12644. Epub 2022 Mar 17. PMID: 35297561; PMCID: PMC9073922.
[11] Hashimoto, K. Detrimental effects of COVID-19 in the brain and therapeutic options for long COVID: The role of Epstein–Barr virus and the gut–brain axis. Mol Psychiatry (2023). https://doi.org/10.1038/s41380-023-02161-5
[12] Seo Won Shin, kI Hyun Cho, Panax ginseng as a potential therapeutic for neurological disorders associated with COVID-19; Toward targeting inflammasome, Journal for Ginseng Research 74 (2023) 23-32
[13] Karosanidze I, Kiladze U, Kirtadze N, Giorgadze M, Amashukeli N, Parulava N, Iluridze N, Kikabidze N, Gudavadze N, Gelashvili L, Koberidze V, Gigashvili E, Jajanidze N, Latsabidze N, Mamageishvili N, Shengelia R, Hovhannisyan A, Panossian A. Efficacy of Adaptogens in Patients with Long COVID-19: A Randomized, Quadruple-Blind, Placebo-Controlled Trial. Pharmaceuticals (Basel). 2022 Mar 11;15(3):345. doi: 10.3390/ph15030345. PMID: 35337143; PMCID: PMC8953947.
[14] Yang J, Lim KH, Lim KT, Woods JT, Mohabbat AB, Wahner-Roedler DL, Ganesh R, Bauer BA. Complementary and alternative medicine for long COVID: a systematic review of randomized controlled trials. Ther Adv Chronic Dis. 2023 Oct 11;14:20406223231204727. doi: 10.1177/20406223231204727. PMID: 37841213; PMCID: PMC10571674.
[15] https://www.kenhub.com/en/library/anatomy/the-vagus-nerve
[16] James McKinlay, Vicki Williamson, Systems thinking simplified – four primary concepts, in The Art of People Management in Libraries, 2010, https://www.sciencedirect.com/topics/computer-science/dynamic-equilibrium
[17] Giulia Muzio, Leslie O’Bray, Karsten Borgwardt, Biological network analysis with deep learning, Briefings in Bioinformatics, Volume 22, Issue 2, March 2021, Pages 1515–1530, https://doi.org/10.1093/bib/bbaa257
[18] Nugraha RV, Ridwansyah H,Ghozali M, Khairani A,F Atik N. Traditional herbal alternative medicine; Traditional medicine candidates as complementary treatments for COVID-19, Evidence-based complementary and alternative medicine, 2020. p. 2020.
[19] Panossian, Alexander, and Thomas Brendler. “The Role of Adaptogens in Prophylaxis and Treatment of Viral Respiratory Infections.” Pharmaceuticals (Basel, Switzerland) vol. 13,9 236. 8 Sep. 2020, doi:10.3390/ph13090236
[20] Tesch, F. et al. Incident autoimmune diseases in association with a SARS-CoV-2 infection: a matched cohort study. Preprint at medRxiv https://doi.org/10.1101/2023.01.25.23285014 (2023).
[21] Yin JX, Agbana YL, Sun ZS, Fei SW, Zhao HQ, Zhou XN, Chen JH, Kassegne K. Increased interleukin-6 is associated with long COVID-19: a systematic review and meta-analysis. Infect Dis Poverty. 2023 Apr 24;12(1):43. doi: 10.1186/s40249-023-01086-z. PMID: 37095536; PMCID: PMC10123579.
[22] Harris E. Severe COVID-19 Linked to Enduring Immune System Changes. JAMA. 2023;330(11):1030.doi:10.1001/jama.2023.16109
[23] Potere N, Del Buono MG, Caricchio R, Cremer PC, Vecchié A, Porreca E, Dalla Gasperina D, Dentali F, Abbate A, Bonaventura A. Interleukin-1 and the NLRP3 inflammasome in COVID-19: Pathogenetic and therapeutic implications. EBioMedicine. 2022 Nov;85:104299. doi: 10.1016/j.ebiom.2022.104299. Epub 2022 Oct 6. PMID: 36209522; PMCID: PMC9536001.
[24] Seo Won Shin, kI Hyun Cho, Panax ginseng as a potential therapeutic for neurological disorders associated with COVID-19; Toward targeting inflammasome, Journal for Ginseng Research 74 (2023) 23-32
[25] Panossian A, Efferth T. Network Pharmacology of Adaptogens in the Assessment of Their Pleiotropic Therapeutic Activity. Pharmaceuticals (Basel). 2022 Aug 25;15(9):1051. doi: 10.3390/ph15091051. PMID: 36145272; PMCID: PMC9504187.
[26] Seo EJ, Klauck SM, Efferth T, Panossian A. Adaptogens in chemobrain (Part II): Effect of plant extracts on chemotherapy-induced cytotoxicity in neuroglia cells. Phytomedicine. 2019 May;58:152743. doi: 10.1016/j.phymed.2018.11.004. Epub 2018 Nov 6. PMID: 30901664.
[27] Alexander G. Panossian, Adaptogens in Mental and Behavioral Disorders, Psychiatric Clinics of North America, Volume 36, Issue 1, 2013, Pages 49-64, ISSN 0193-953X, ISBN 9781455771479, https://doi.org/10.1016/j.psc.2012.12.005.
[28] Seo EJ, Klauck SM, Efferth T, Panossian A. Adaptogens in chemobrain (Part I): Plant extracts attenuate cancer chemotherapy-induced cognitive impairment – Transcriptome-wide microarray profiles of neuroglia cells. Phytomedicine. 2019 Mar 1;55:80-91. doi: 10.1016/j.phymed.2018.10.022. Epub 2018 Oct 19. PMID: 30668446.
[29] Kaur P, Robin, Makanjuola VO, Arora R, Singh B, Arora S. Immunopotentiating significance of conventionally used plant adaptogens as modulators in biochemical and molecular signalling pathways in cell mediated processes. Biomed Pharmacother. 2017 Nov; 95:1815-1829. Epub 2017 Oct 6.
[30] Karosanidze I, Kiladze U, Kirtadze N, Giorgadze M, Amashukeli N, Parulava N, Iluridze N, Kikabidze N, Gudavadze N, Gelashvili L, Koberidze V, Gigashvili E, Jajanidze N, Latsabidze N, Mamageishvili N, Shengelia R, Hovhannisyan A, Panossian A. Efficacy of Adaptogens in Patients with Long COVID-19: A Randomized, Quadruple-Blind, Placebo-Controlled Trial. Pharmaceuticals (Basel). 2022 Mar 11;15(3):345. doi: 10.3390/ph15030345. PMID: 35337143; PMCID: PMC8953947.






Excellent information, and research, Donnie. Thank you for the work that you do!
Thank you! As usual, well spoken thought out information. Tried and true, the herbs stand together in integrity! Thank God for the natural world and for you Donnie, bless you for your long standing endurance and solid understanding!