In the attempt to tame the COVID-19 virus, scientists around the world are working to understand how the disease is spread and how best to approach prevention and treatment. But with the avalanche of information we’re presented with every day, it’s easy to come away with more questions than answers.
There are a couple of recent findings that stand out as particularly important. One relates to the method of transmission, and the other to individual susceptibility to the disease.
The Dominant Route of Transmission
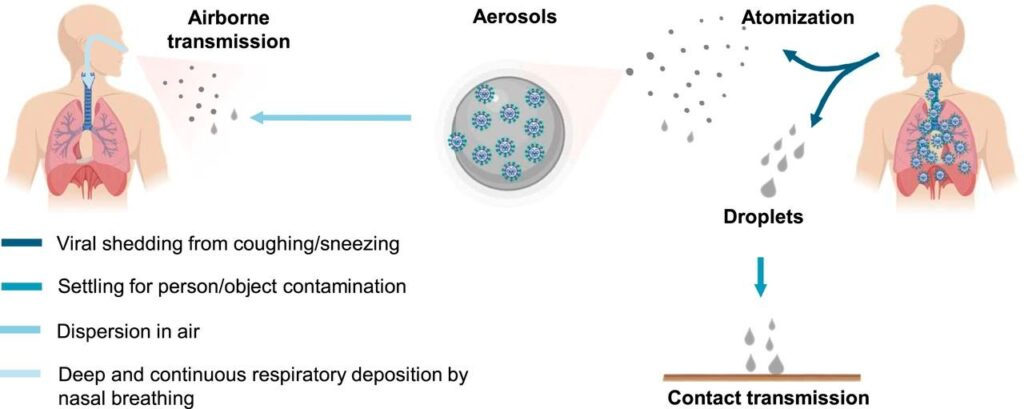
I know people who spend a great deal of time sanitizing cardboard boxes and every piece of mail that enters their home. But airborne transmission, particularly via aerosols from human atomization (coughs, sneezes, and even talking), is highly virulent and is the dominant route for the transmission of COVID-19.
Several parameters likely influence the microorganism survival and airborne delivery, including temperature, humidity, microbial resistance to external physical and biological stresses, and solar ultraviolet (UV) radiation.[1]
A recent finding showed that the highest viral load in the upper respiratory tract occurs at the onset of symptoms. This suggests that the peak of infectiousness occurs on or before symptom onset and that there is substantial asymptomatic transmission for SARS-CoV-2.[2]
This is concerning, because although the WHO and the US Centers for Disease Control and Prevention (CDC) have emphasized excessive hand washing and sanitizing to prevent contact transmission, they have largely ignored the role of airborne transmission.[3]
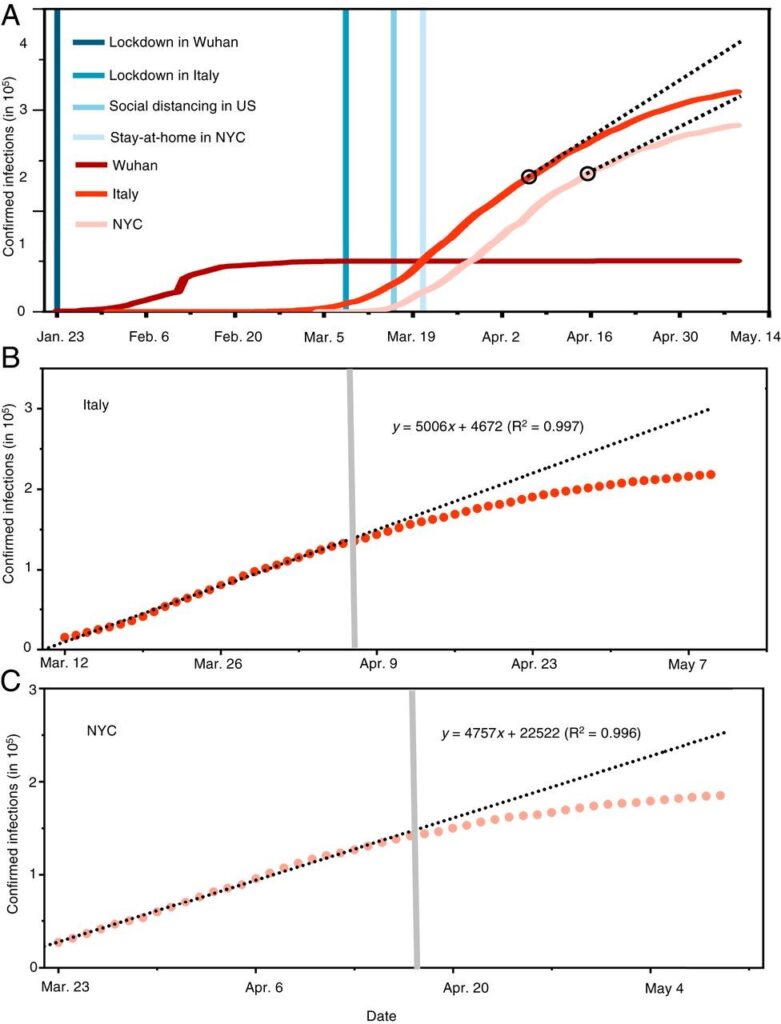
Although we’ve received conflicting information from government officials and scientists about whether or not facemasks are helpful for preventing the spread of the virus, new analysis reveals that the difference with and without mandated face covering is the determining factor in shaping the trends of the pandemic. The data is clear: Using a facemask significantly reduces the number of infections.
Identifying the Most Susceptible
While COVID-19 can infect virtually everyone in the human population, only about 5% are susceptible to a severe infection. These are the patients that end up in intensive care and are also those who are much more likely to die from the disease. In general, people who are more likely to suffer from severe infection can be identified on the basis of comorbid medical conditions or age.
People most at risk for severe infection are individuals 85 years of age and older, or those with comorbid conditions, including preexisting respiratory and cardiovascular disease, immunocompromised status, morbid obesity, diabetes mellitus, and possibly significant kidney or liver impairment.[4]
It makes sense to keep in place stringent safeguards to protect those who are vulnerable. This requires the entire population to continue practicing good hygiene, social distancing, and mask wearing, while simultaneously focusing on sheltering the vulnerable population until adequate ‘herd’ immunity has been achieved. This will be accomplished through natural exposure or with the addition of a SAFE and effective vaccine, which may not be available for a year or longer.
Blood Type as a Risk Factor
A study of patients in China discovered an association between ABO blood type and COVID-19 infection status by comparing COVID-19 patients with the general population. People with blood group A have a significantly higher risk for acquiring COVID-19 compared with non-A blood groups, whereas blood group O has a significantly lower risk for the infection compared with non-O blood groups.[5]
A number of subsequent studies have found the same association. In an initial study of 265 patients with COVID, the authors observed that blood group O individuals were significantly under‐represented among patients who required hospitalization for severe COVID‐19 infection. Conversely, blood group A was significantly more common in patients with severe COVID‐19 compared to the local population. Subsequently, in a larger validation cohort that included 2153 patients with COVID‐19, this ABO effect was reproduced with blood group O again being associated with a significant protective effect.[6]
Another report, which analyzed the data of almost 2,000 patients hospitalized for COVID-19 in Italy and Spain, found that those with type A blood were at increased risk for respiratory failure. Type O blood, on the other hand, was found to have a protective effect.[7]
Finally, an analysis of healthcare data of 1559 individuals tested for COVID-19 found a higher proportion of blood group A and a lower proportion of blood group O among COVID patients. Researchers concluded that the effect of blood type is not explained by other risk factors including age, sex, hypertension, diabetes mellitus, overweight status, and chronic cardiovascular and lung disorders.[8]
Why Are Older People More Susceptible to the Virus?
When considering those who suffer severe effects from the virus, we have to consider comorbidity, not just age. The number one reason that older people tend to suffer more serious effects from COVID-19 is that older adults are more likely to have long-term health problems that can put them at risk. It’s important to keep in mind that there is a difference between chronological age and biological age.
Older people are more likely to have underlying health conditions, such as cardiovascular disease, lung conditions, diabetes and cancer. It is these complications, not just age, that dictate the severity of COVID-19 in individuals.[9] Data from China shows that such comorbidities dramatically increase the risk of dying from COVID-19.[10]
Older adults in general have weaker immune systems. Some of this is the result of poor nutritional status, such as a lack of adequate vitamin D and zinc (for more in-depth information, see my blogs on vitamin D and zinc). Lung tissue loses elasticity with age, making respiratory diseases like COVID-19 a particular concern for older people. Older adults often have increased inflammatory and oxidative stress, and this environmental terrain is much more conducive to COVID-19 related organ system damage.
Studies show that neutrophilic inflammation contributes to the higher mortality of COVID-19 in patients with underlying co-morbidities such as diabetes and cardiovascular diseases.[11],[12]
“Deaths of Despair” Increase with Social Isolation

By continuing to stay at home and avoid social contact, the resulting isolation and despair may increase overall mortality and will certainly negatively affect quality-of-life. Numerous scientific studies on the adverse health consequences of social isolation suggest that we are on the brink of a potentially devastating mental health crisis that will increase the death toll from COVID-19.[13]
Social isolation increases the risk for “deaths of despair,” including suicide or drug overdose, as well as deaths from other causes like heart disease and cancer. People will die from COVID-19, and some will succumb to the adverse effects of the social distancing that is so vital to slowing the spread of the infection. We have to strike a balance and we have to weigh the risk-to-benefit ratio. Above all, we need to focus on health promotion, rather than disease management.
Older adults need to socialize, and they benefit from face-to-face interaction perhaps more than any other age group. A recent study published in the American Journal of Preventive Medicine showed that adults over the age of 50 who volunteer for at least 100 hours a year—approximately two hours per week—experienced a large reduction in their risk of developing physical limitations and their risk of death. They also had higher physical activity levels and an improved sense of well-being compared to those who didn’t volunteer.[14]
Nourishing the Root – The Foundation of Wholistic Health

A recent meta-analysis evaluating the effectiveness of herbal medicines for managing the symptoms of COVID-19 found that combining herbal medicine with Western medicine significantly improved symptoms caused by the virus, including cough, sore throat, and fatigue.15
In the quest to find a cure for the pandemic, I’m grateful that the humble remedies offered by nature are being recognized as valuable partners in healing. If this virus has taught us anything, it is that general health optimization is what really matters. Healing is not just about your immune system, or any one part of the body. Healing is about WHOLENESS and total VITALITY.
All systems are connected, and this is why the
foundation of what I do is to build robustness, enhance auto-regulation and
auto-organization, and support adaptation and protection through herbal and
nutritional support that is gentle, non-specific, and multi-faceted.
[1] Zhang, R., et al., Formation of urban fine particulate matter. Chem. Rev. 115, 3803–3855 (2015).
[2] He X., et al., Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26, 672–675
[3] Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19 [published online ahead of print, 2020 Jun 11]. Proc Natl Acad Sci U S A. 2020;202009637. doi:10.1073/pnas.2009637117
[4] Preskorn SH. The 5% of the Population at High Risk for Severe COVID-19 Infection Is Identifiable and Needs to Be Taken Into Account When Reopening the Economy. J Psychiatr Pract. 2020;26(3):219-227. doi:10.1097/PRA.0000000000000475
[5] Zhao, Jiao, ewt. Al., Relationship between the ABO Blood Group and the COVID-19 Susceptibility, DO – 10.1101/2020.03.11.20031096
[6] O’ Sullivan, Jamie, et. al., More on ‘Association between ABO blood groups and risk of SARS-CoV-2 pneumonia’, British Journal of Haematology · May 2020, DO – 10.1111/bjh.16845
[7] Ellinghaus, D., et. al., The ABO blood group locus and a chromosome 3 gene cluster associate with SARS-CoV-2 respiratory failure in an Italian-Spanish genome-wide association analysis, medRxiv 2020.05.31.20114991; doi: https://doi.org/10.1101/2020.05.31.20114991
[8] Zietz M, Tatonetti NP. Testing the association between blood type and COVID-19 infection, intubation, and death. medRxiv. 2020;2020.04.08.20058073. Published 2020 Apr 11. doi:10.1101/2020.04.08.20058073
[9] Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis [published correction appears in Lancet Infect Dis. 2020 Apr 15;:] [published correction appears in Lancet Infect Dis. 2020 May 4;:]. Lancet Infect Dis. 2020;20(6):669-677
[10] Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639-645. doi:10.1016/j.jinf.2020.03.019
[11] Tomar B, Anders HJ, esai J, Mulay SR. Neutrophils and Neutrophil Extracellular Traps Drive Necroinflammation in COVID-19. Cells. 2020;9(6):E1383. Published 2020 Jun 2. doi:10.3390/cells9061383
[12] Barnes BJ, Adrover JM, Baxter-Stoltzfus A, et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J Exp Med. 2020;217(6):e20200652. doi:10.1084/jem.20200652
[13] National Academies of Sciences, Engineering, and Medicine. 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, DC: The National Academies Press. https://doi.org/10.17226/25663.
[14] Kim, ES., et. al., Volunteering and Subsequent Health and Well-Being in Older Adults: An Outcome-Wide Longitudinal Approach, Am J Prev Med 2020;000(000):1−11.
15 Ang L, Song E, Lee HW, Lee MS. Herbal Medicine for the Treatment of Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2020;9(5):1583. Published 2020 May 23. doi:10.3390/jcm9051583

This is the most comprehensive article on risk factors for COVID-19 that I have read. Grateful for your research/evaluation/communication skills Donnie. Presented with clarity and hope. Natural medicine has an important place in this journey!
Thank you!
Very concise and informative. Thanks for your research and commentary.
Thank You so very much – very easy to read and understand – and very thorough!!!
I would like to be included in all of your email communications to your consumers.
Donnie, so well researched, and so informative. I hope this could find it’s way to main-stream media as we need more well-thought analysis like this. It provides hope, but also real understanding, which helps us navigate this crisis more effectively. Thanks!