Cancer is a major concern and is on the rise worldwide, including among younger people in the United States. However, many people don’t think about the relationship between glutamine supplementation and cancer, even though it’s a complex and evolving topic.
What Makes Cancer Cells Different?
Cancer cells display a high metabolic adaptability. This allows them to flourish in fluctuating microenvironmental conditions. While normal cells die in challenging conditions, cancer cells are able to continue their metabolic activities to ensure their ongoing survival.
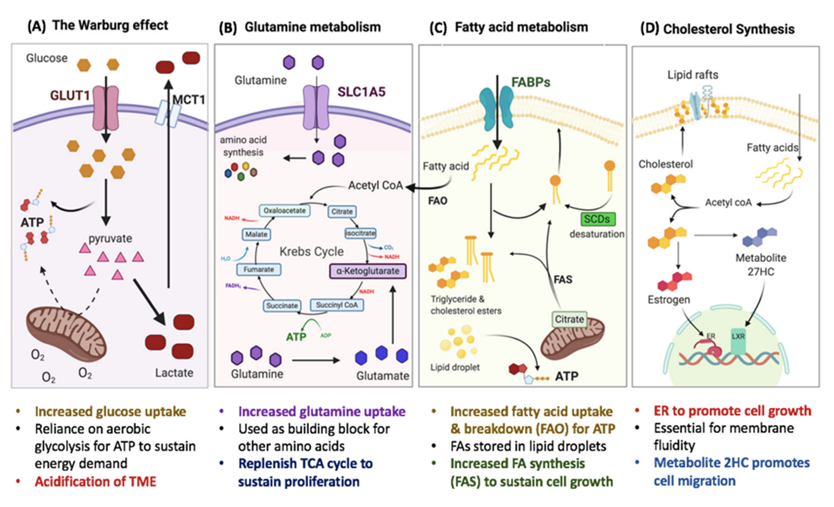
To adapt metabolically, cancer cells use glucose, glutamine, and lactate. These three—glucose, glutamine, and lactate—are among their major metabolic substrates.[1]
A tumor is a mass of tissue. Some are cancerous and some are benign. Cancerous tumors display reprogrammed metabolic activities that promote cancer progression.
Metabolic phenotypes (characteristics) in tumors are both heterogeneous and flexible. These phenotypes result from the combined effects of many different factors, some intrinsic to the cancer cell (for the medical doctors and science-minded among my readers, this includes cell lineage, differentiation state, and somatically-acquired mutations) and others imposed by the microenvironment (these include nutrient milieu, interactions with the extracellular matrix, and stromal cells).
What is Glutamine?
Glutamine is the most abundant free amino acid in the body. It is held within skeletal muscle cells. Our cells use glutamine for both bioenergetic and biosynthetic needs.
Glutamine is also the main substrate for DNA and fatty acid synthesis. It reduces oxidative stress by stimulating glutathione synthesis, stops the process of cancer cachexia (erosion of lean muscle mass, also termed wasting syndrome), and nourishes the immune system and the intestinal epithelium (lining of the gut).[2]
Once a cell takes up glutamine, most of it is converted to glutamate. This is done by mitochondrial glutaminase, an enzyme whose levels are frequently upregulated (higher) in tumors and tumor cell lines.[3],[4]
Conceptually, this information suggests that dietary and supplemental glutamine should be limited. That appears to make sense from a biochemical perspective.
But that said, there’s a hitch.
Glutamine Supplementation May Help Fight Cancer
The truth is that oral glutamine does NOT appear to increase cancer growth. Not only that, glutamine supplementation is associated with a host of health-promoting benefits.
Cancer cells exhibit dysregulation of the enzymes involved in the key regulatory steps of glucose transport, glycolysis, tricarboxylic acid (TCA) cycle, and glutaminolysis (again, for those who want the scientific details, the glutaminolysis that is governed not only by oncogenes such as c-MYC but also by hypoxia-inducible factor-1 and loss of function of the p53 tumor suppressor gene).
The MYC oncogene serves a critical role in numerous types of human cancers. It is considered a master regulator of cell metabolism and proliferation, reprogramming mitochondrial metabolism towards sustaining cellular viability and the TCA cycle.[5]
A Controversial Topic
The issue at hand is the growing controversy surrounding the use of glutamine supplementation for cancer patients. This controversy arises from the fact that cancer cells use glutamine as a source of energy alongside glucose.
However, avoiding oral glutamine is unnecessary.
This is complicated—and involves quite a bit of biochemistry—but let me explain.
Rapid cellular proliferation, which is what cancer cells do, is metabolically demanding. It necessitates large supplies of macro-nutrients.
However, the full complement of amino acids is rarely accessible to cancer cells. Lacking amino acids, these cells must leverage available substrates to re-balance the amino acid supply-and-demand network.[6]
The most abundant circulating amino acid is glutamine. Glutamine is not only a versatile substrate for cellular energy and proliferation but also facilitates the uptake of other amino acids, nucleotide synthesis, pH balance, redox balance, signaling, and detoxification.[7]
Cancer Cells Have a “Glutamine Addiction”
Many cancer cells show increased glutamine uptake and glutamine dependence, so much so that some scientists describe cancer cells as having a “glutamine addiction.”[8]
Cancer cells consume excessive glutamine, roughly 50-fold greater than the amount required for protein synthesis and 7-fold greater than the next most consumed amino acids (i.e., serine, leucine) in one study.[9] Keep in mind that only about 6% of cell mass is made from glutamine.[10]
Triple-negative Breast Cancer Cells Use Glutamine
Glutamine consumption is especially pronounced in the triple-negative breast cancer (TNBC) subtype. These cells are distinguished by their upregulated expression of key genes related to using glutamine. In addition, they are sensitive[JM1] [JY2] to drugs that inhibit glutamine-related pathways, which makes these drugs effective for controlling this type of cancer.[11],[12]
“Central to this process (of some tumor cell types) is the use of glutamine to drive acetyl-CoA oxidation through a series of amine exchanges, potentially a way to boost TCA cycle fluxes by harnessing nutrient gradients,” explain a team of Australian scientists that studied glutamine promoting glucose oxidation in TNBC and published their findings in 2022 in the peer-reviewed journal Oncogene.
“This elevates glucose oxidation in TNBC cells, but only when glutamine is available. Our work introduces a specific TCA cycle, which we term ‘single-pass glutaminolysis,’ to describe a single round of glutamine TCA cycle traversal that facilitates glucose catabolism. Phenotyping tumors for a rigid glucose-glutamine metabolic coupling as a vulnerability marker holds the potential for accurate identification of tumors sensitive to the inhibition of glutamine uptake and/or metabolism.”[13]
Glutamine metabolism is a key regulator of epigenetic modifications in cancer stem cells (CSC).
Glutamine has been shown to modulate CSC fate in different tissues, directly or indirectly. Cancer stem cells exhibit a complex response to glutamine variations.[14]
In particular, specific tumor-initiating cells expressing high cell surface levels of stem marker CD9 are capable of metabolic reprogramming and activating glutamine.[15]
Oral Glutamine Is Not the Problem
Oral glutamine has no impact on the metabolic reprogramming and hijacking of glutamine by cancer cells.
Now, here’s the most important thing to keep in mind: the majority of glutamine consumed in the diet is retained by cells in the intestinal mucosa.
That means it does not reach the circulation.
This suggests that oral glutamine has no impact on glutamine transport supplied from a direct source of glutamine. This observation is supported by at least two separate studies.[16],[17]
Nonetheless, with all this cellular metabolic insight, you might think that cancer patients should avoid glutamine supplementation.
However, I have not found any research that demonstrates glutamine supplementation induces or promotes cancer.
Where the confusion lies is in the fact that the proteins c-MYC, and sometimes KRAS (one of the RAS protein family members that are often mutated in cancer cells), drive cell division at elevated levels in more than half of all cancers. These proteins are able to pull glucose and glutamine from the cancer cells’ micro-environment (the area around the tumor) to use for energy.
Still, this isn’t the fault of glutamine.
Cancer Controls the Local Environment and has Complex Energy Needs
Instead of blaming glutamine, it has to do with the cancer’s ability to control the local environment.
So, although cancer cells have increased use of glutamine to fuel anabolic processes, supplementing with oral glutamine does not facilitate this process.
In fact, supplementing with oral glutamine might actually inhibit cancer growth. In other words, glutamine supplementation may help fight cancer.
Cancer’s Complex Energy Needs
Cancer cells need to take glutamine from the environment outside of the cell; but if that area is deprived of glutamine, the cancer cells adapt and find a way to continue to grow and multiply. Glutamine is the most abundant amino acid in the human bloodstream, so it makes complete sense that cancer cells would find a way to utilize it.
Cancer cells actually find a way to manipulate the micro-environment to produce glutamine and they also compete with tumor‐associated T lymphocytes for glutamine. The increased utilization of glutamine nitrogen in nucleotide production is facilitated by growth‐promoting signals. For instance, the oncogene c‐MYC can induce cancer cell glutamine energy activation. Keep in mind cancer cells are completely capable of adapting to a low glutamine environment, which is part of cancer-associated cachexia or wasting syndrome.
Oral Glutamine Has No Effect on Cancer’s Ability to Hijack Cellular Glutamine
Plasma concentration of glutamine is low in many patients with critical illness. A low level of plasma glutamine is an independent risk factor for mortality.
A low plasma glutamine concentration is the best indicator of glutamine depletion.
We know that skeletal muscle is the major producer of glutamine and that a part of the profound depletion of skeletal muscle seen in critical illness reflects the need to produce glutamine.[18]
Oral glutamine restores decreased levels of glutathione that are often depleted in cancer patients as a result of undergoing conventional treatments such as chemotherapy and radiotherapy[JM3] [JY4] . It facilitates regeneration processes of the intestine epithelium and immunological system.[19]
In a DMBA-breast cancer animal model, oral glutamine down-regulated c-MYC, up-regulated tumor suppressor p53 signaling, and inhibit Akt signaling. It was found to be extremely useful for increasing the effectiveness of cancer treatments.[20]
In addition, a recent study showed that oral glutamine reduced radiation morbidity in breast cancer and was associated with the increased expression of a novel serum protein biomarker.[21]Finally, another study showed that patients receiving radiation who do not receive glutamine can develop severe malnutrition and mucositis when compared with those receiving it.[22]
Glutamine Supplementation: Glutamine is an Indispensable Nutrient in Oncology
Several studies, in both humans and laboratory animals, have shown that oral, enteral, or intravenous glutamine supports the metabolism of the tumor-bearing host and can ameliorate gastrointestinal toxicity caused by cancer treatments.
A growing body of scientific literature shows that topical and oral glutamine are the preferred routes for this amino acid to promote mucosal healing during and after cancer treatment.[23]
Within the last four decades, dozens of human clinical studies have evaluated oral glutamine’s safety and side effects in various patient groups.
Evidence supports the benefit of oral (enteral) glutamine to reduce symptoms and improve and/or maintain the quality of life of cancer patients.
The benefits of glutamine supplementation include not only improved overall nutritional status, but also decreased mucosal damage (mucositis, stomatitis, pharyngitis, esophagitis, and enteritis).
Numerous studies in patients receiving glutamine-enriched parenteral nutrition or oral for several weeks confirmed the clinical safety of this approach in a catabolic patient population.
In addition, nitrogen retention appears to be enhanced when glutamine is administered.[24]
In the great majority of these clinical studies, glutamine supplementation in cancer patients improves host metabolism and clinical situation without increasing tumor growth. Glutamine enhances the effectiveness of chemotherapy while reducing its toxic side effects. [25],[26],[27],[28],[29],[30],[31]
We have also seen that oral glutamine supplementation can help reduce acute radiation toxicities and help with too much weight loss. [32]
A 2021 meta-analysis found that oral glutamine supplementation had therapeutic benefits in preventing and ameliorating radiation-induced oral mucositis among patients with head and neck cancer.[33]
A Super Immune Nutrient
It’s not an exaggeration to say that oral glutamine is a super-immune nutrient.
Glutamine is a key nutrient for immune health and is essential for the production of glutathione.[34]
It has been shown to ameliorate treatment-related toxicity, augment treatment efficacy, and improve quality of life in cancer patients while even extending life as well.[35],[36]
How I use Glutamine
I don’t recommend glutamine to cancer patients[JM5] [JY6] as a single supplement.
Instead, I use it in various formulations.
The primary formula I use for general immune health, as well as recovery for those who are depleted, is glutamine combined with a non-denatured whey protein, colostrum, and a unique form of creatine chelated to magnesium. This provides the body with a readily available source of magnesium, while also making the creatine more active by protecting it from cyclization. This patented mineral amino acid chelate contributes to an overall positive impact on many functions including, but not limited to, a non-steroidal anabolic enhancing effect, while also providing rehydration and endurance to a person showing signs of physiological stress.[37],[38]
For gastrointestinal health specifically, I combine glutamine with other essential herbal extracts and nutrients such as Aloe vera, DGL licorice, Lemon balm, Chamomile, mastic gum, and potassium bicarbonate.
About the Author:
Donald R. Yance is the founder of the Mederi Center. A Clinical Master Herbalist and Certified Nutritionist, Donnie is renowned for his extraordinary knowledge and deep understanding of the healing properties of plants and nutrition, as well as of epigenetics, laboratory medicine, oncologic pathology, and molecular oncology. He is a professional member of the American Herbalists Guild, National Association of Nutrition Professionals, Academy of Integrative Health and Medicine, and the Society for Integrative Oncology.
References:
[1] Jhudit Perez-Escuredo, Rajesh K Dadhich, Suveera Dhup, Andrea Cacace, Vincent F Van Hee, Christophe J De Saedeleer, Martina Sboarina, Fabien Rodriguez, Marie-Josephine Fontenille, Lucie Brisson, Paolo E Porporato, and Pierre Sonveaux , Lactate promotes glutamine uptake and metabolism in oxidative cancer cells, CELL CYCLE 2016, VOL. 15, NO. 1, 72–83 http://dx.doi.org/10.1080/15384101.2015.1120930
[2] Michalak KP1, Maćkowska-Kędziora A2, Sobolewski B3, Woźniak P3. Key Roles of Glutamine Pathways in Reprogramming the Cancer Metabolism, Oxid Med Cell Longev. 2015;2015:964321. doi: 10.1155/2015/964321. Epub 2015 Oct 25.
[3] DeBerardinis RJ, Cheng T. Q’s next: The diverse functions of glutamine in metabolism, cell biology and cancer. Oncogene. 2010;29:313–324. doi: 10.1038/onc.2009.358.
[4] Levine AJ, Puzio-Kuter AM. The control of the metabolic switch in cancers by oncogenes and tumor suppressor genes. Science. 2010;330:1340–1344. doi: 10.1126/science.1193494.
[5] Papanikolopoulou A, Syrigos N, Vini L, Papasavva M, Lazopoulos G, Kteniadakis S, Spandidos DA, Charpidou A, Drakoulis N. Use of oral glutamine in radiation-induced adverse effects in patients with thoracic and upper aerodigestive malignancies: Results of a prospective observational study. Oncol Lett. 2022 Jan;23(1):19. doi: 10.3892/ol.2021.13137. Epub 2021 Nov 16. PMID: 34858523; PMCID: PMC8617560.
[6] Vettore L, Westbrook RL, Tennant DA. New aspects of amino acid metabolism in cancer. Br J Cancer. 2020;122:150–6.
[7] DeBerardinis RJ, Mancuso A, Daikhin E, Nissim I, Yudkoff M, Wehrli S, et al. Beyond aerobic glycolysis: transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proc Natl Acad Sci USA. 2007;104:19345–50.
[8] Le A, Lane AN, Hamaker M, Bose S, Gouw A, Barbi J, et al. Glucose-independent glutamine metabolism via TCA cycling for proliferation and survival in B cells. Cell Metab. 2012;15:110–21.
[9] Jain M, Nilsson R, Sharma S, Madhusudhan N, Kitami T, Souza AL, et al. Metabolite profiling identities a key role for glycine in rapid cancer cell proliferation. Science. 2012;336:1040–4.
[10] Hosios AM, Hecht VC, Danai LV, Johnson MO, Rathmell JC, Steinhauser ML, et al. Amino acids rather than glucose account for the majority of cell mass in pro- liferating mammalian cells. Dev Cell. 2016;36:540–9.
[11] Gross MI, Demo SD, Dennison JB, Chen L, Chernov-Rogan T, Goyal B, et al. Antitumor activity of the glutaminase inhibitor CB-839 in triple-negative breast cancer. Mol Cancer Therapeutics. 2014;13:890–901.
[12] Quek LE, van Geldermalsen M, Guan YF, Wahi K, Mayoh C, Balaban S, Pang A, Wang Q, Cowley MJ, Brown KK, Turner N, Hoy AJ, Holst J. Glutamine addiction promotes glucose oxidation in triple-negative breast cancer. Oncogene. 2022 Aug;41(34):4066-4078. doi: 10.1038/s41388-022-02408-5. Epub 2022 Jul 18. PMID: 35851845; PMCID: PMC9391225.
[13] Quek LE, van Geldermalsen M, Guan YF, Wahi K, Mayoh C, Balaban S, Pang A, Wang Q, Cowley MJ, Brown KK, Turner N, Hoy AJ, Holst J. Glutamine addiction promotes glucose oxidation in triple-negative breast cancer. Oncogene. 2022 Aug;41(34):4066-4078. doi: 10.1038/s41388-022-02408-5. Epub 2022 Jul 18. PMID: 35851845; PMCID: PMC9391225.
[14] Pacifico F, Leonardi A, Crescenzi E. Glutamine Metabolism in Cancer Stem Cells: A Complex Liaison in the Tumor Microenvironment. Int J Mol Sci. 2023 Jan 25;24(3):2337. doi: 10.3390/ijms24032337. PMID: 36768660; PMCID: PMC9916789.
[15] Wang V.M., Ferreira R.M.M., Almagro J., Evan T., Legrave N., Zaw Thin M., Frith D., Carvalho J., Barry D.J., Snijders A.P., et al. CD9 identifies pancreatic cancer stem cells and modulates glutamine metabolism to fuel tumour growth. Nat. Cell Biol. 2019;21:1425–1435. doi: 10.1038/s41556-019-0407-1
[16] Biolo G., Fleming R.Y., Maggi S.P., Wolfe R.R. Transmembrane transport and intracellular kinetics of amino acids in human skeletal muscle. Am. J. Physiol. Metab. 1995;268:E75–E84.
[17] Wu G. Intestinal mucosal amino acid catabolism. J. Nutr. 1998;128:1249–1252.
[18] Wernerman, Jan, Glutamine supplementation, Wernerman Annals of Intensive Care 2011, 1:25 http://www.annalsofintensivecare.com/content/1/1/25
[19] Michalak KP, Maćkowska-Kędziora A, Sobolewski B, Woźniak P. Key Roles of Glutamine Pathways in Reprogramming the Cancer Metabolism, Oxid Med Cell Longev. 2015;2015:964321. doi: 10.1155/2015/964321. Epub 2015 Oct 25.
[20] R. Salehi-Tabar, L. Nguyen-Yamamoto, L. E. Tavera-Mendoza, T. Quail, V. Dimitrov,B. An, L. Glass, D. Goltzman, J. H. White, Vitamin D receptor as a master regulator of the c-MYC/MXD1 network, Proc Natl Acad Sci U S A. 2012 Nov 13;109(46):18827-32. doi: 10.1073/pnas.1210037109. Epub 2012 Oct 29.
[21] V.K. Todorova, Y. Kaufmann, S. Luo, V.S. Klimberg, Modulation of p53 and c-myc in DMBA-induced mammary tumors by oral glutamine. Nutr Cancer. 2006;54(2):263-73.
[22] I. Rubio, L.J. Suva, V. Todorova, S. Bhattacharyya, Y. Kaufmann, A. Maners, M. Smith, V.S. Klimberg, Oral Glutamine Reduces Radiation Morbidity in Breast Conservation Surgery. JPEN J Parenter Enteral Nutr. 2013 Feb 6.
[23] Anderson PM, Lalla RV. Glutamine for Amelioration of Radiation and Chemotherapy Associated Mucositis during Cancer Therapy. Nutrients. 2020;12(6):E1675. Published 2020 Jun 4. doi:10.3390/nu12061675.
[24] Ziegler TR, Benfell K, Smith RJ, Young LS, Brown E, Ferrari-Baliviera E, Lowe DK, Wilmore DW. Safety and metabolic effects of L-glutamine administration in humans. JPEN J Parenter Enteral Nutr. 1990 Jul-Aug;14(4 Suppl):137S-146S. doi: 10.1177/0148607190014004201.
[25] Rouse, K, Nwokedi, E, Woodliff, JE, Epstein, J, and Klimberg, VS: Glutamine enhances selectivity of chemotherapy through changes in glutathione metabolism. Ann Surg 221 420-426, 1995.
[26] Jacobs, DO, Evans, A, O’Dwyer, ST, Smith, RJ, and Wilmore, DW:Disparate effects of 5-fluorouracil on the ileum and colon of enterally fed rats with protection by dietary glutamine. Surg Forum 38 45-47, 1987.
[27] Andrews FJ Griffiths RD. Glutamine: essential for immune nutrition in the critically ill. Br J Nutr 2002;87:S3-S8.
[28] Rouse, K, Nwokedi, E, Woodliff, JE, Epstein, J, and Klimberg, VS: Glutamine enhances selectivity of chemotherapy through changes in glutathione metabolism. Ann Surg 221 420-426, 1995.
[29] Klimberg, VS, Nwokedi, E, Hutchins, LF, Pappas, AA, Lang, NP, et al.: Glutamine facilitates chemotherapy while reducing toxicity. JPEN J Parent Enteral Nutr 16 83S-87S, 1992
[30] Rouse, K, Nwokedi, E, Woodliff, JE, Epstein, J, and Klimberg, VS: Glutamine enhances selectivity of chemotherapy through changes in glutathione metabolism. Ann Surg 221 420-426, 1995.
[31] Yoshida, S, Matsui, M, Shirouzu, Y, Fujita, H, Yamana, H, et al.: Effects of glutamine supplements and radiochemotherapy on systemic immune and gut barrier function in patients with advanced esophageal cancer. Ann Surg 227 485-491, 1998
[32] Papanikolopoulou A, Syrigos N, Vini L, Papasavva M, Lazopoulos G, Kteniadakis S, Spandidos DA, Charpidou A, Drakoulis N. Use of oral glutamine in radiation-induced adverse effects in patients with thoracic and upper aerodigestive malignancies: Results of a prospective observational study. Oncol Lett. 2022 Jan;23(1):19. doi: 10.3892/ol.2021.13137. Epub 2021 Nov 16. PMID: 34858523; PMCID: PMC8617560.
[33] Alsubaie HM, Alsini AY, Alsubaie KM, Abu-Zaid A, Alzahrani FR, Sayed S, Pathak AK, Alqahtani KH. Glutamine for prevention and alleviation of radiation-induced oral mucositis in patients with head and neck squamous cell cancer: Systematic review and meta-analysis of controlled trials. Head Neck. 2021 Oct;43(10):3199-3213. doi: 10.1002/hed.26798. Epub 2021 Jul 9. PMID: 34240498.
[34] Zhang J, Pavlova NN, Thompson CB. Cancer cell metabolism: the essential role of the nonessential amino acid, glutamine. EMBO J. 2017 May 15;36(10):1302-1315. doi: 10.15252/embj.201696151. Epub 2017 Apr 18. PMID: 28420743; PMCID: PMC5430235.
[35] Wang CC, Hwang TZ, Yang CC, Lien CF, Wang CC, Shih YC, Yeh SA, Hsieh MC. Impact of Parenteral Glutamine Supplement on Oncologic Outcomes in Patients with Nasopharyngeal Cancer Treated with Concurrent Chemoradiotherapy. Nutrients. 2022 Feb 26;14(5):997. doi: 10.3390/nu14050997. PMID: 35267972; PMCID: PMC8912271.
[36] Chang SC, Lai YC, Hung JC, Chang CY. Oral glutamine supplements reduce concurrent chemoradiotherapy-induced esophagitis in patients with advanced non-small cell lung cancer. Medicine (Baltimore). 2019 Feb;98(8):e14463. doi: 10.1097/MD.0000000000014463
[37] Brilla, L.R., FACSM, Giroux, M.S. Taylor, A. Kennedy, J. Ramierex, R.E. Puz, D. and Knutzen, K.M. FACSM. Magnesium-Creatine Supplementation on Total Body Water, ICF and ECF Compartments, Western Washington University, WA. American College Sports Medicine 2002
[38] Brilla, L.R. Giroux, M. Taylor, A. Knutzen, K., Magnesium-Creatine chelate supplementation may allow runners to reach their physiological threshold later in exercise, Nutrition Week 2002 supplement to the February issue of the American Journal of Clinical Nutrition (75, 2(S), 2002)

As always, thanks for the great insight from your posts!